Lower-income patients to get higher subsidies for cost-effective surgical implants
Sign up now: Get ST's newsletters delivered to your inbox

The new Implant Subsidy List and enhanced subsidies for implants will mean lower out-of-pocket payments.
PHOTO ILLUSTRATION: ST FILE
SINGAPORE – From Dec 1, 2023, patients who need surgical implants such as high-cost replacement heart valves, hearing devices, intraocular lenses for cataracts, or knee replacement implants can get higher means-tested subsidies, and not be subjected to a dollar cap.
These are among the bulk of commonly used implants in public healthcare institutions that will be included in a new Implant Subsidy List, which will kick in on the same day, said Ministry of Health (MOH) officials at a media briefing on Nov 29. They have been assessed by MOH’s Agency for Care Effectiveness (ACE) to be clinically effective and cost-effective.
MOH said lower-income patients who need high-cost implants will benefit most from the changes.
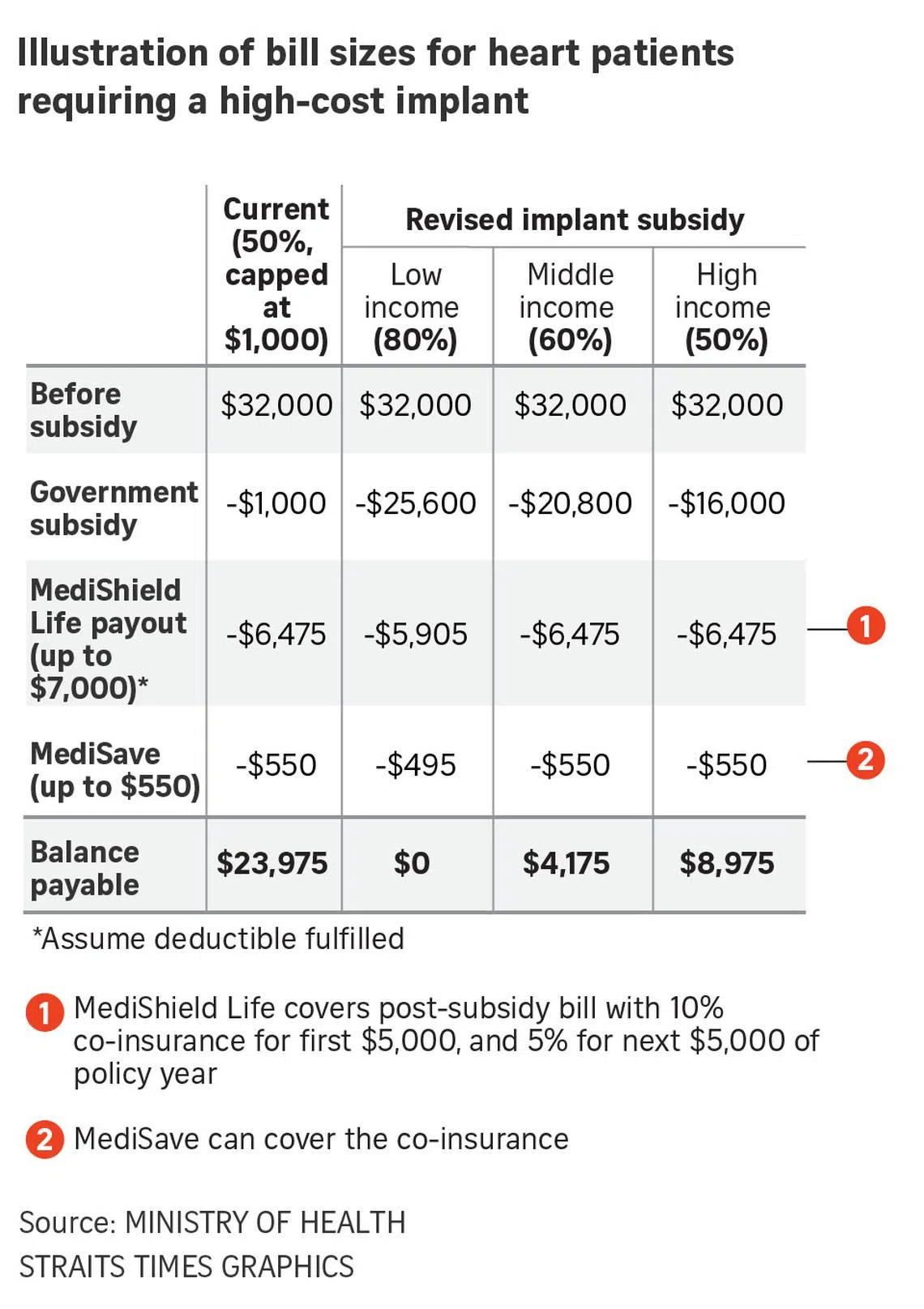
Currently, patients in B2 to C wards and day surgery settings receive subsidies for all implants, with Singapore citizens getting up to a 50 per cent subsidy, capped at $1,000. Singapore permanent residents (PRs) get up to a 25 per cent subsidy, with a cap of $500.
Because of this, manufacturers have little incentive to reduce their prices as all their implants are eligible for subsidy, MOH said.
ACE has found that there can be a big variation in the prices offered here and abroad, and prices of implants can even vary across Singapore hospitals.
The new Implant Subsidy List is similar in part to the Cancer Drug List
With the new list, implants are no longer automatically eligible for subsidy, and this facilitates negotiations with manufacturers for more competitive prices, MOH said.
An earlier pilot subsidy list for three types of implants for heart patients and hearing implants resulted in price reductions of up to 25 per cent and savings of around $8.3 million over 2017 to 2022, MOH said.
The changes, made to ensure that healthcare cost growth remains sustainable, come as the use of implants, which has increased over the years, is expected to rise further with a rapidly ageing population.
MOH also expects newer and higher-cost implants to come on the market quickly.
From 2013 to 2021, implant spending in public healthcare institutions grew from $93 million to $163 million, according to MOH data. Increasing implant charges and the rising volume of implant procedures contributed to this, said an MOH spokesperson.
There is a wide range of implants used here, including pacemakers for those with an abnormally slow heart rate, treatment implants to help reduce eye pressure for those with glaucoma, and hip replacement implants for those with osteoarthritis of the hip joint.
Having a list means that Singaporeans who meet the criteria for items on it will receive between 50 per cent and 80 per cent subsidy in class B2 and C wards and day surgery settings, depending on their means-test level, with no dollar cap.
Singapore PRs will get a 25 per cent to 50 per cent subsidy in these settings, also with no dollar cap, MOH said.
There are no changes to MediShield Life, MediSave and Integrated Shield Plan coverage for implants, so patients can continue to tap these schemes, whether or not the implant they need is on the new list.
MOH said it will review the financing coverage of these schemes at a later juncture.
It said that about 8 per cent of the volume of implants used at public healthcare institutions have been found to be not clinically effective and cost-effective, and they will not be in the new list.
Generally, the majority of the unlisted implants will have a suitable subsidised alternative on the new list. If not, patients may consider non-implant treatment options, MOH said.
The 15 categories in the new list include cardiac implantable electronic devices such as pacemakers, cochlear implants, which are hearing devices that bypass the damaged parts of the inner ear to stimulate the remaining auditory nerve fibres, and hip, knee and sports medicine implants.
Another 11 categories, including spine implants and mammary implants, are currently under assessment and will progressively move to the list by the end of 2025.
In the meantime, the implants in the 11 categories will be eligible for current capped subsidies, MOH said.
Associate Professor Yeo Khung Keong, chief executive of the National Heart Centre Singapore, said the new subsidy framework will ensure that the right patients get the subsidies, and encourage implant manufacturers to lower their prices because only competitively priced products will be included in the list. These savings can then be passed on to patients.
“In the public sector, we already have a high level of support. Cardiology has a special medical service package that helps address the needs of patients who need life-saving, high-cost implants such as pacemakers or defibrillators,” said Prof Yeo.
“I think this is an attempt to do even more, to cover more costly items that are not already covered, such as replacement heart valves costing $30,000 to $40,000 that a group of patients may need.”
The Implant Subsidy List will supersede the special medical service package, which has been around for about two decades and offers up to 65 per cent to 80 per cent subsidies for implants for B2 to C class patients.
Prof Yeo said some of the newer technology that has surfaced in the past few years is not included in the package, but the new list will cover it, benefiting needy patients.
Overall, the list will result in better prices for patients as implants that are uncompetitively priced will be excluded, if similarly effective technology exists, he said.
“They may be a bit more fancy or branded, but there are alternatives that can do the job as well.” said Prof Yeo.



