Using AI to detect breast cancer that doctors miss
Sign up now: Get ST's newsletters delivered to your inbox

A patient gets a mammogram at Bacs-Kiskun County Hospital in Hungary on Feb 20, 2023.
PHOTO: NYTIMES
KECSKEMET, Hungary – Inside a dark room at Bacs-Kiskun County Hospital outside Budapest, Dr Eva Ambrozay, a radiologist with more than two decades of experience, peered at a computer monitor showing a patient’s mammogram.
Two radiologists had previously said the X-ray did not show any signs that the patient had breast cancer.
But Dr Ambrozay was looking closely at several areas of the scan circled in red, which artificial intelligence (AI) software had flagged as potentially cancerous.
“This is something,” she said. She soon ordered the woman to be called back for a biopsy, which is taking place within the next week.
Advancements in AI are beginning to deliver breakthroughs in breast cancer screening by detecting the signs that doctors miss.
So far, the technology is showing an impressive ability to spot cancer at least as well as human radiologists, according to early results and radiologists, in what is one of the most tangible signs to date of how AI can improve public health.
Hungary, which has a robust breast cancer screening programmes, is one of the largest testing grounds for the technology on real patients.
At five hospitals and clinics that perform more than 35,000 screenings a year, AI systems were rolled out starting in 2021 and now help to check for signs of cancer that a radiologist may have overlooked.
Clinics and hospitals in the United States, Britain and the European Union are also beginning to test or provide data to help develop the systems.
AI usage is growing as the technology has become the centre of a Silicon Valley boom, with the release of chatbots such as ChatGPT showing how AI has a remarkable ability to communicate in human-like prose – sometimes with worrying results.
Built off a similar form used by chatbots that is modelled on the human brain, the breast cancer screening technology shows other ways that AI is seeping into everyday life.
Widespread use of the cancer detection technology still faces many hurdles, doctors and AI developers said.
Additional clinical trials are needed before the systems can be more widely adopted as an automated second or third reader of breast cancer screens, beyond the limited number of places now using the technology.

Hungary has become a major testing ground for AI software to spot cancer.
PHOTO: NYTIMES
The tool must also show it can produce accurate results on women of all ages, ethnicities and body types. And the technology must prove it can recognise more complex forms of breast cancer and cut down on false positives that are not cancerous, radiologists said.
The AI tools have also prompted a debate about whether they will replace human radiologists, with makers of the technology facing regulatory scrutiny and resistance from some doctors and health institutions.
For now, those fears appear overblown, with many experts saying the technology will be effective and trusted by patients only if it is used in partnership with trained doctors.
And ultimately, AI could be lifesaving, said Dr Laszlo Tabar, a leading mammography educator in Europe who said he was won over by the technology after reviewing its performance in breast cancer screening from several vendors.
“I’m dreaming about the day when women are going to a breast cancer center and they are asking, ‘Do you have AI or not?’” he said.
Hundreds of images a day
In 2016, Professor Geoff Hinton, one of the world’s leading AI researchers, argued the technology would eclipse the skills of a radiologist within five years.
“I think that if you work as a radiologist, you are like Wile E Coyote in the cartoon,” he told The New Yorker in 2017.
“You’re already over the edge of the cliff, but you haven’t yet looked down. There’s no ground underneath.”
Prof Hinton and two of his students at the University of Toronto built an image recognition system that could accurately identify common objects such as flowers, dogs and cars.
The technology at the heart of their system – called a neural network – is modelled on how the human brain processes information from different sources.
It is what is used to identify people and animals in images posted to apps such as Google Photos, and allows Siri and Alexa to recognise the words people speak. Neural networks also drove the new wave of chatbots such as ChatGPT.
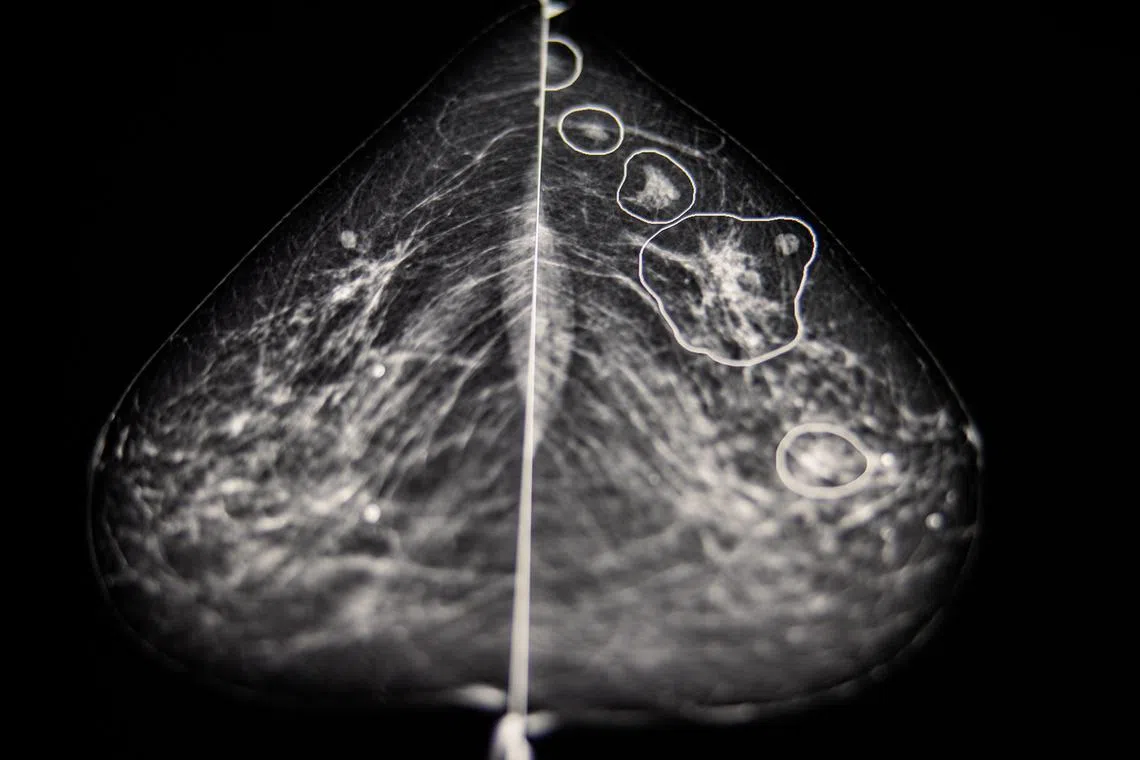
Possible anomalies in a breast cancer screen are highlighted by an AI software at the Bacs-Kiskun County Hospital.
PHOTO: NYTIMES
Many AI evangelists believed such technology could easily be applied to detect illness and disease, such as breast cancer in a mammogram.
In 2020, there were 2.3 million breast cancer diagnoses and 685,000 deaths from the disease, according to the World Health Organisation.
But not everyone felt replacing radiologists would be as easy as Prof Hinton predicted.
Dr Peter Kecskemethy, a computer scientist who co-founded Kheiron Medical Technologies, a software company that develops AI tools to assist radiologists detect early signs of cancer, knew the reality would be more complicated.
Dr Kecskemethy grew up in Hungary, spending time at one of Budapest’s largest hospitals.
His mother was a radiologist, which gave him a first-hand look at the difficulties of finding a small malignancy within an image. Radiologists often spend hours every day in a dark room looking at hundreds of images and making life-altering decisions for patients.
“It’s so easy to miss tiny lesions,” said Dr Edith Karpati, Dr Kecskemethy’s mother, who is now a medical product director at Kheiron.
“It’s not possible to stay focused.”

Founder of Kheiron Medical Technologies Peter Kecskemethy, and his mother, radiolost. Edith Karpati.
PHOTO: NYTIMES
Dr Kecskemethy, along with Kheiron’s co-founder, Mr Tobias Rijken, an expert in machine learning, said AI should assist doctors.
To train their AI systems, they collected more than five million historical mammograms of patients whose diagnoses were already known, provided by clinics in Hungary and Argentina, as well as academic institutions, such as Emory University.
The company, which is in London, also pays 12 radiologists to label images using special software that teaches the AI to spot a cancerous growth by its shape, density, location and other factors.
From the millions of cases the system is fed, the technology creates a mathematical representation of normal mammograms and those with cancers.
With the ability to look at each image in a more granular way than the human eye, it then compares that baseline to find abnormalities in each mammogram.
Last year, after a test on more than 275,000 breast cancer cases, Kheiron reported that its AI software matched the performance of human radiologists when acting as the second reader of mammography scans.
It also cut down on radiologists’ workloads by at least 30 per cent because it reduced the number of X-rays they needed to read.

Director of MaMMa Klinika Andras Vadászy, The technology is showing an impressive ability to spot cancer as well as human radiologists.
PHOTO: NYTIMES
In other results from a Hungarian clinic last year, the technology increased the cancer detection rate by 13 per cent because more malignancies were identified.
The National Cancer Institute has estimated that about 20 per cent of breast cancers are missed during screening mammograms.
Dr Constance Lehman, a professor of radiology at Harvard Medical School and chief of breast imaging and radiology at Massachusetts General Hospital, urged doctors to keep an open mind.
“We are not irrelevant,” she said, “but there are tasks that are better done with computers.”
At Bacs-Kiskun County Hospital outside Budapest, Dr Ambrozay said she had initially been sceptical of the technology – but was quickly won over.
She pulled up the X-ray of a 58-year-old woman with a tiny tumour spotted by the AI that Dr Ambrozay had a hard time seeing.
The AI saw something, she said, “that seemed to appear out of nowhere”. NYTIMES