BRANDED CONTENT
This medical school trains clinician-scientists ready to create tech-led biomedical innovations
State-of-the-art learning strategies, access to cutting-edge tools and mentoring by world-class faculty equip Duke-NUS Medical School’s graduates with the right skill sets to solve healthcare problems of tomorrow
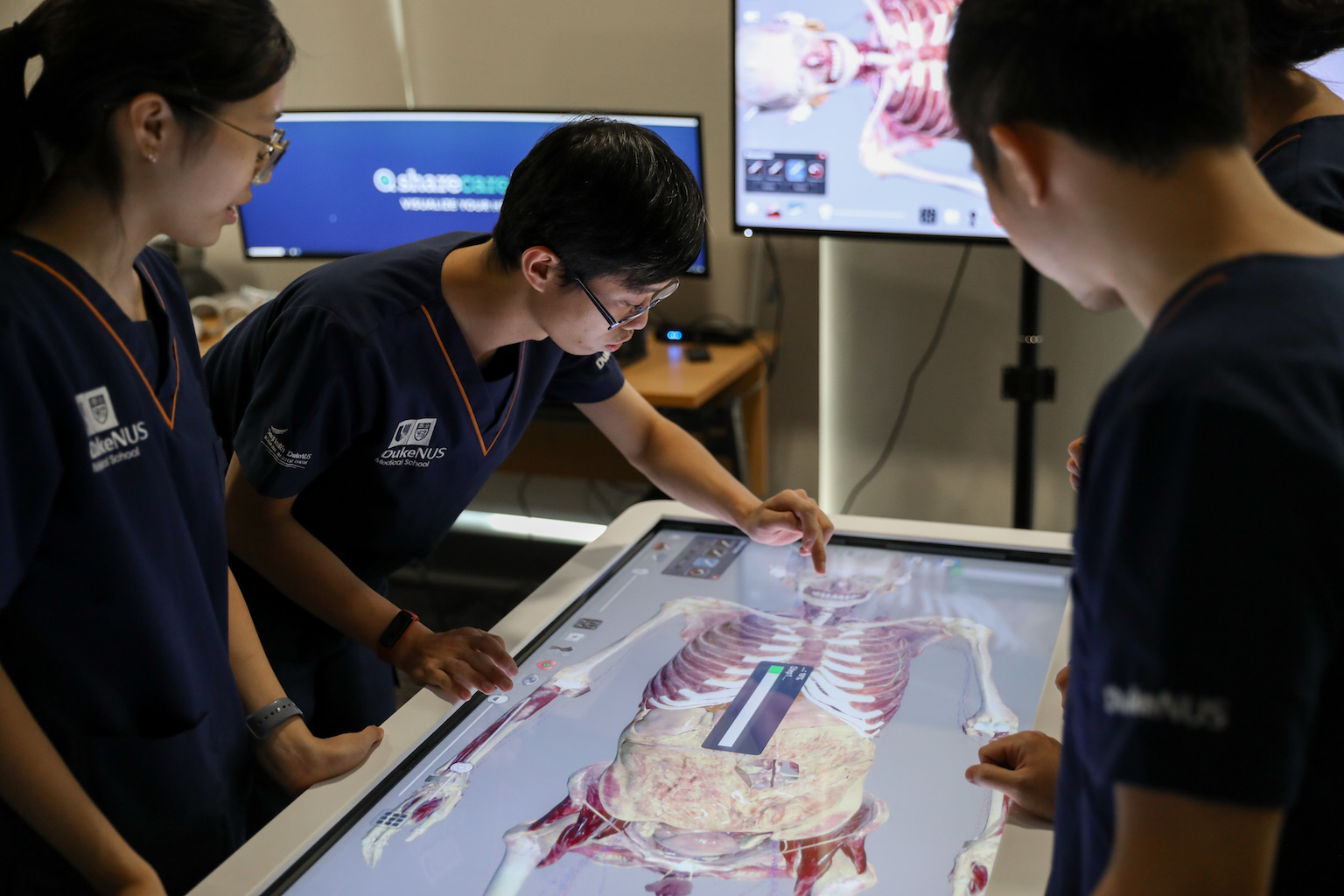
Duke-NUS Medical School’s new Immersive Learning Space is equipped with state-of-the-art technology such as virtual dissection tables.
PHOTO: DUKE-NUS MEDICAL SCHOOL
When Dr Petty Chen was experimenting with using radio-frequency identification (RFID) wristbands – or patient tags – to more accurately map out in-demand services within Sengkang General Hospital, she never thought it would one day be used to keep patients safe during Covid-19.
The tags were initially designed to relay data about patients’ locations to a central computer system in order to optimise the hospital’s ability to manage manpower and other resources by calculating patient turnover rates, including admissions, discharges and transfers between wards.
However, the tags had an unexpected purpose during the pandemic: contact tracing.
“With patient tags, we could monitor the distance between patients and the duration that they had been together,” explains Dr Chen. “This allowed us to do contact tracing very easily in the hospital. So, if there was one infected patient, we didn’t have to quarantine an entire ward.”
This is an example of how thoughtful technology-led innovation can help resolve emerging healthcare problems – and precisely why Duke-NUS Medical School is, more than ever, inculcating this spirit of innovation in its graduates (in line with the Ministry of Education’s emphasis on technology-enabled and technology-enriched learning in higher education).
Today, several challenges loom on the horizon for healthcare: an ageing population, steadily increasing healthcare costs and insufficient manpower, to name a few.
To tackle the industry’s growing demands, Duke-NUS is training a new generation of clinician-scientists who do not only rely on existing clinical knowledge but are also able to think out of the box and harness technological expertise in order to innovate more effective solutions for a myriad of healthcare issues.
Inspiring new ways of thinking
One of the key ways it is doing so is with the new Innovation and Design Thinking module, under the Doctor of Medicine (MD) programme.
Spearheaded by Dr Chen herself, the week-long course trains budding physicians to develop a solutions-oriented mindset to address existing healthcare challenges by using what she calls “design frameworks” – a creative problem-solving approach that enables students to more fully understand key healthcare problems before collectively brainstorming solutions.
The complex and multi-layered nature of issues in healthcare requires clinicians to approach them from multiple perspectives. However, tunnel vision is one of the largest obstacles that clinicians may face when attempting to brainstorm solutions, particularly in more experienced consultants, says Dr Chen, who is also director of medical products at Asus Global.
She explains that this happens because clinicians may often approach a problem without having a holistic understanding of it: “You only really see one side of things as a doctor. You may see something one way, but the nurses could see another, and the patient could report something entirely different.”

The module, which is now in its third year, thus aims to nurture the right mindset in students from the start and empower them to become more adept clinicians in the future. Through the course, students are tasked to fully evaluate a wide variety of healthcare challenges – such as the most efficient means to distribute contraceptives or how to improve screening for elderly patients with diabetic ulcerations.
The latter, for instance, requires students to understand what exactly causes elderly patients to miss or avoid their screenings, even if the consequences of leaving ulcerations untreated can be severe?
Once students have a better understanding of the problem from the patient’s perspective – such as a lack of knowledge about their medical condition, or a tendency to forget their appointments – they can then understand where the patient lies relative to other stakeholders such as caregivers and regulatory bodies.
From there, they can harness the use of medical technology to craft a more holistic solution that takes all of these perspectives into account to address the concerns of different stakeholders and improve the quality of care.
Using innovative technologies in the classroom
If students are to think up technology-enabled solutions, they also have to be familiar with – and comfortable operating at – the cutting edge of medical technology.
To achieve this, Duke-NUS offers access to state-of-the-art technologies that are divided into four major categories: Immersive Learning, Simulation and Serious Gaming, 3D Printing, and Artificial Intelligence and Learning Analytics.
This includes trials with Augmented Reality and Virtual Reality technologies that allow students to practise and better familiarise themselves with anatomy by immersing them in more accurate and detailed simulations.

Duke-NUS students are given many hands-on opportunities to use advanced technology like Virtual Reality simulations in their research.
PHOTO: DUKE-NUS MEDICAL SCHOOL
“These approaches aim to support and enhance our MD curriculum, help develop new educational approaches, insights and technological innovations to transform medical education, and so improve lives,” says Professor Fernando Bello, associate dean of the Technology Enhanced Learning & Innovation Department in the Duke-NUS Office of Education.
For instance, the school has constructed a new Immersive Learning Space equipped with 3D high-definition virtual dissection tables and customisable anatomical models to facilitate students’ self-directed learning.
3D printing is also being used to create realistic patient-specific models in order to better familiarise students with human anatomy and pathology, allowing them to perform more accurate clinical interventions.
In training its students to develop, pilot, test and modify possible technology-based solutions, Duke-NUS aims to produce clinicians who are technology creators, not just technology consumers, says Prof Bello.
All this is done in line with Duke-NUS’ “Clinician First, Clinician Plus” educational philosophy – the idea that graduates will be first and foremost excellent clinicians, and grow into leading educators, scientists, scholars and innovators over the course of their careers.
Prof Bello says: “By exposing our students to a wide range of new technologies, and facilitating and supporting their use across the curriculum, we are preparing them not only to be avid and able users of technology, but also to drive technological innovation in healthcare.”
“Growing healthcare demands require new, creative, and disruptive approaches,” he says. “An innovation culture that includes innovation for educating doctors, and innovation for delivering and receiving care, is fundamental to successfully tackling existing and future healthcare challenges.”
Want to be part of Duke-NUS Medical School’s culture of innovation? Click here to sign up for their virtual open house on May 21.



