Private insurers and hospitals all tied up in a knot; MOH helping to untie it: Ong Ye Kung
Sign up now: Get ST's newsletters delivered to your inbox
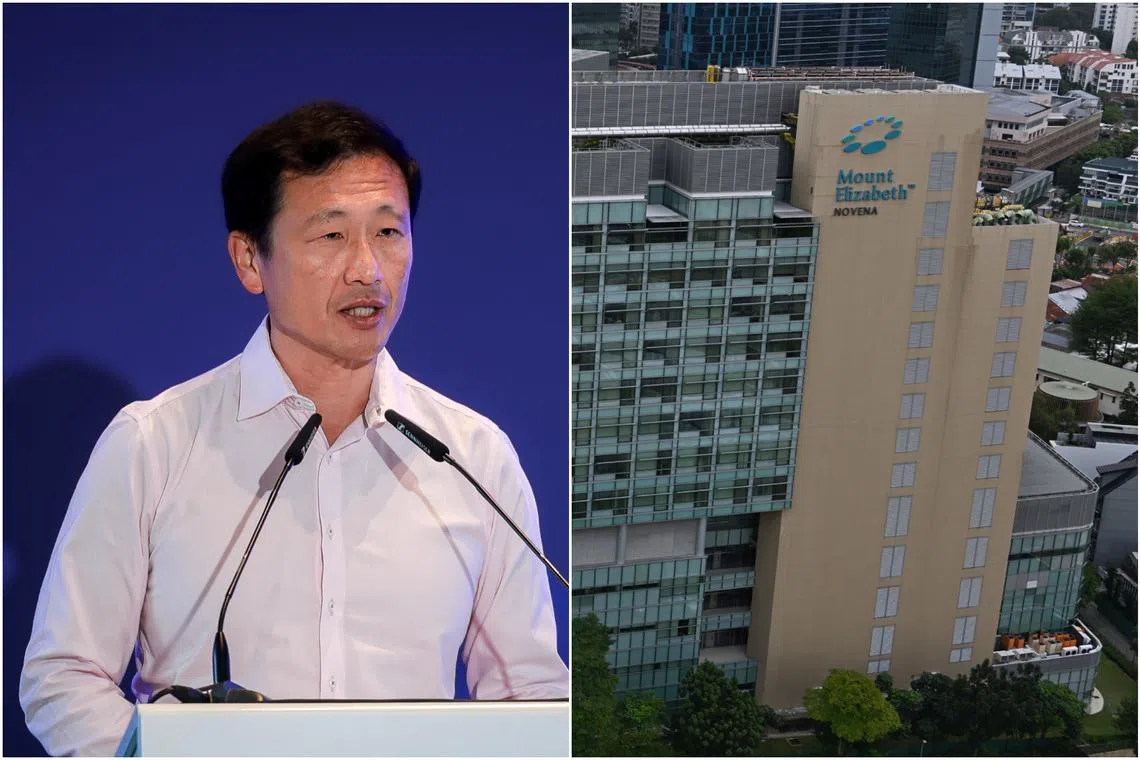
Health Minister Ong Ye Kung was providing the Health Ministry’s perspective in light of Great Eastern's recent suspension of the issuance of pre-authorisation certificates for admissions to Mount Elizabeth Hospital and Mount Elizabeth Novena Hospital.
ST PHOTOS: GAVIN FOO, CHONG JUN LIANG
Follow topic:
SINGAPORE – Private health insurers and private hospitals have got themselves tied up in a knot, to the detriment of all stakeholders including patients, said Health Minister Ong Ye Kung on July 1.
“I have been expressing my concern about the state of private insurance and private healthcare for some time. The current trend is not sustainable,” he said in a Facebook post.
Mr Ong was providing the Health Ministry’s perspective in the light of Great Eastern (GE) insurance group’s recent suspension on the issuance of pre-authorisation certificates
“The recent moves by insurers may be disconcerting, but we need to see them against this broader context and the need to set the private healthcare financing system on a more sustainable footing. Otherwise, everyone loses,” he said, adding that the Ministry of Health (MOH) will be facilitating the untying of the knot.
GE had said it has temporarily stopped issuing pre-authorisation certificates for the two hospitals from June 17, citing their high costs compared with other private hospitals as the reason.
A pre-authorisation certificate confirms that the insurer has approved the medical treatment, including the costs, before the treatment begins. The certificate may cover the cost of the procedure, medications and other related expenses. Patients who are policyholders have a clear understanding of the costs that will be covered, reducing the risk of unexpected medical bills.
Mr Ong stressed that the GE issue affects patients on private insurance plans who intend to receive care at private hospitals. In Singapore, more than 90 per cent of acute inpatient care is delivered in public hospitals, including those who opt for unsubsidised wards. Patients of public hospitals are not affected by GE’s latest actions.
Explaining how the knot came about, Mr Ong said a big factor lay in insurance design.
“Insurers know that policyholders are worried about incurring an unexpected huge hospital bill, so they launch insurance products that offer generous coverage to win customers and market share. These include ‘as-charged’ or no-limit coverage, and riders that will protect almost to the last dollar,” he said.
However, when someone else is footing almost the entire medical bill, the healthcare provider-patient dynamic changes, and there is the tendency to use more than what is necessary.
The likelihood of a patient with a rider making a claim is 1.4 times that of a patient without; and the size of the claim is also, on average, 1.4 times that of a patient without riders, he said.
As insurance claims escalate, the premiums can no longer cover these claims, and insurers have responded in two ways:
Introducing safeguards such as having panel doctors and, more recently, suspending pre-authorisation for selected hospitals;
Raising premiums.
Premiums for riders have risen sharply over the past few years and, as a result, many policyholders, especially seniors, have terminated their rider policies when they realise that it is not worth paying almost $10,000 or more every year, he said.
Policyholders are also unhappy that they are paying rising premiums, especially when there are more restrictions. Meanwhile, healthcare providers are finding it more cumbersome to make claims, while insurers are struggling to stay viable for their health portfolios.
“As for (the) Government, with all these developments, we can see that more patients with private insurance are opting for subsidised public healthcare,” Mr Ong said.
“As it is, public healthcare accounts for around 80 per cent of hospital beds in Singapore but provides care for 90 per cent of all inpatients. It will come under increasing pressure.”
MOH has intervened in several ways.
It introduced fee benchmarks in 2018 to guide pricing and guard against overcharging.
Today, more than 90 per cent of cases fall within the surgeon fee benchmarks, compared with 80 per cent in 2018, and the average annual growth in private surgeon fees has moderated from 3 per cent from 2010 to 2018, to 0.4 per cent from 2019 to 2023, Mr Ong said.
“We are now studying the possibility of going beyond professional fees, by introducing more benchmarks for hospital charges, to guide fee setting by private hospitals,” he added.
MOH is also taking action against a small minority of doctors who make errant claims, putting them through a refresher course on fee setting, or even suspending them from claiming from MediSave and MediShield Life.
“We need more private hospital options, especially affordable ones, like Mount Alvernia Hospital. MOH is therefore exploring the possibility of a new not-for-profit private hospital. However, even if the decision is to proceed, this will take a few years,” he said.
Mr Ong admitted that all these actions will not be sufficient and that ultimately, private insurers need to take a hard and realistic look at their product design, particularly that of riders.
“To be fair, they have made some effort. Most insurers offer more affordable rider alternatives, which may not fully cover deductibles or have a bigger co-payment component. The premiums for such alternatives can be half of the premiums for riders with the most generous coverage,” he said.
“More importantly, these riders can help to dull the incentives to over-service and overcharge, while still providing the additional protection against large cash co-payments that policyholders value. It will help focus private hospitals and private doctors on delivering value and ensuring affordability for their patients.”
In the longer term, patients seeking care in private hospitals will find that they are getting a better deal than in the current situation, he said.
“Every stakeholder needs to do its part, so that step by step, this knot can be gradually loosened and untied.”


