Novel cell-based gene therapy developed in Singapore improves lives of cancer-stricken pets
Sign up now: Get ST's newsletters delivered to your inbox

Ms Bridget Low with her 11-year-old toy poodle, Oscar. Tests revealed a 1.5cm tumour in Oscar's left lung.
ST PHOTO: ARIFFIN JAMAR
Follow topic:
SINGAPORE - In early 2020, Ms Bridget Low, 26, noticed a lump in her toy poodle’s neck. A biopsy found the mass cancerous. The dog, Oscar, had also had daily coughing fits.
Further tests revealed a 1.5cm tumour lodged in Oscar’s left lung. Canine lung cancer is rare but deadly, and the 11-year-old poodle was given only three months to live.
But there was a possible lifeline in the form of doggy stem cells carrying cancer-killing genes. The therapy was developed at the National University of Singapore by Associate Professor Too Heng-Phon, Dr Sarah Ho and their team, based on a treatment initially meant for human patients.
The group was instrumental in taking the cure to animal patients, working with a few veterinarians here, including Dr Lee Yee Lin of Gentle Oak Veterinary Clinic.
Oscar is one of 56 dogs and cats with terminal cancer who either lived longer than expected, or had a better quality of life, thanks to the novel treatment developed by the researchers at the NUS Yong Loo Lin School of Medicine (NUS Medicine).
The therapy has two ingredients – the modified stem cells that are injected into the animal, and off-the-shelf anti-fungal drugs taken orally. The researchers developed a technology to insert large amounts of yeast-based genes into the stem cells that would react with the anti-fungal drugs to target the cancer cells.
For Oscar, once the engineered stem cells were injected, they naturally gravitated to the lung tumour and nested on the cancer cells. The dog was then given the anti-fungal pill for four days, as part of one treatment cycle.
The anti-fungal drug entered the stem cells and reacted with the genes inside the cells to morph into a cancer killer called Fluorouracil (5FU).
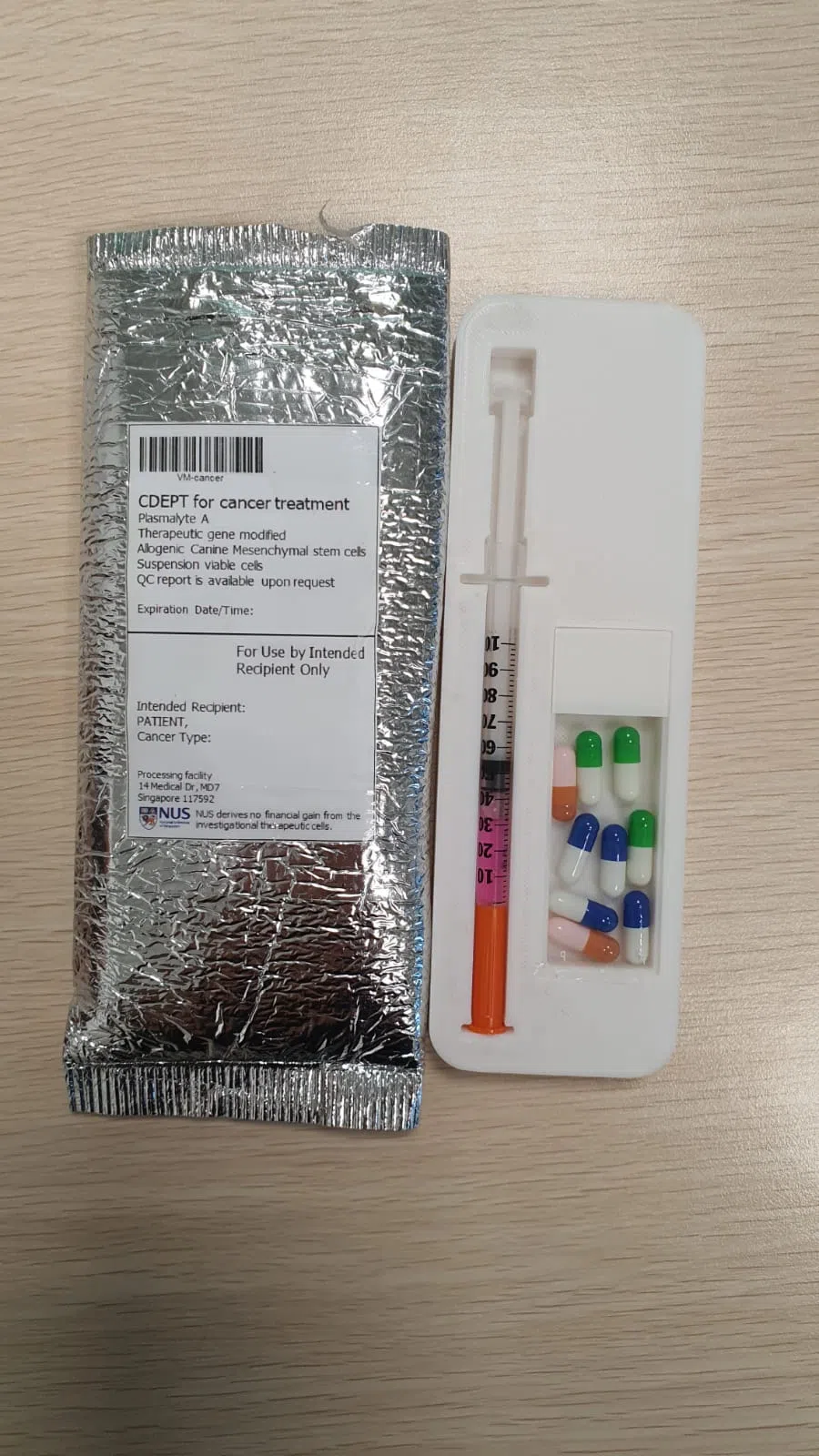
A syringe of the modified, therapeutic stem cells developed by the NUS Medicine researchers.
PHOTO: NUS YONG LOO LIN SCHOOL OF MEDICINE
The modified stem cells act like suicide bombers, loading the toxic 5FU around the tumour to kill it, and eventually dying themselves, said Dr Ho, a senior research fellow at NUS Medicine’s biochemistry department who was involved in the development of the therapy. “It’s a clean system, delivering the therapy and clearing out,” she added.
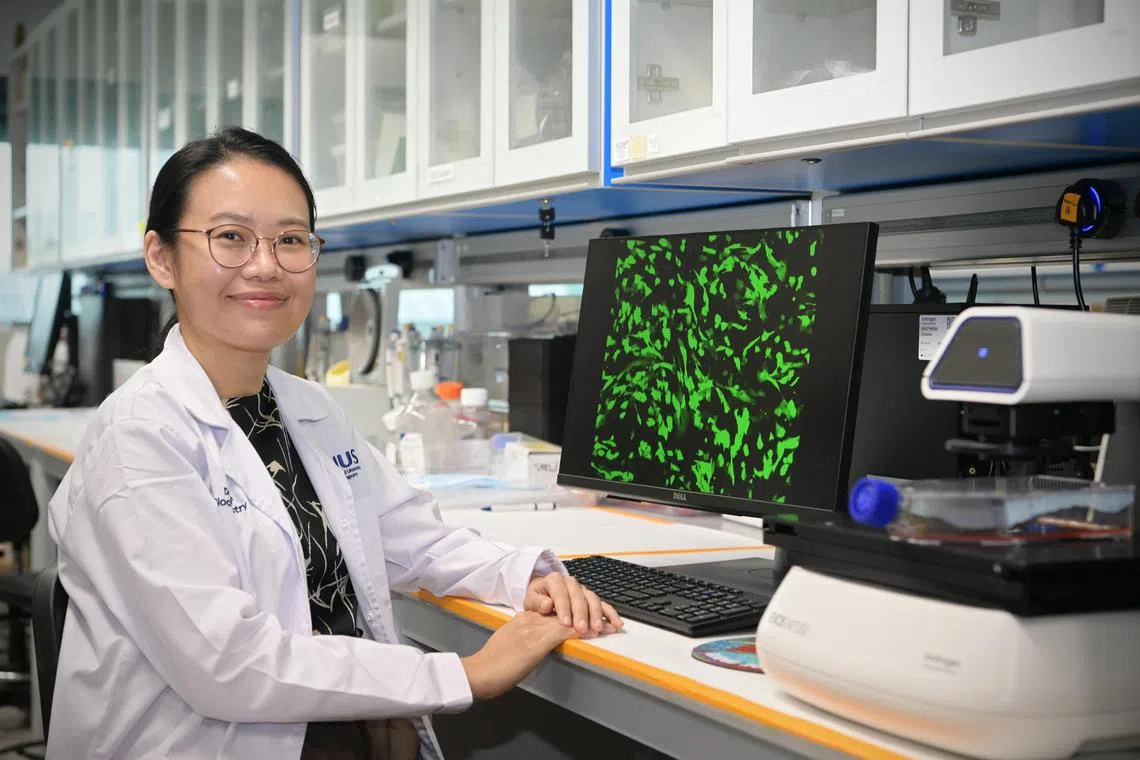
Dr Sarah Ho with microscopic images of the modified, therapeutic stem cells she helped to develop.
ST PHOTO: NG SOR LUAN
Dr Ho’s team was actually working on the therapy to combat aggressive human tumours until a vet, hearing about it, contacted them in 2018.
5FU is commonly used in chemotherapy, and can cause severe side effects such as diarrhoea, bleeding gums and a higher risk of infection. But since the 5FU from the NUS therapy only surrounds the cancer cells, it does not cause serious side effects, though mild ones can occur.
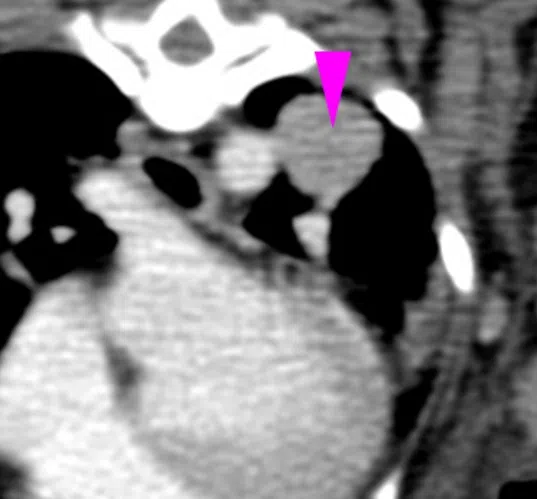
A scan of Oscar’s lung, showing the 1.5cm tumour in his left lung.
PHOTO: NUS YONG LOO LIN SCHOOL OF MEDICINE
Oscar underwent five treatment cycles between March and September 2020, which were free, as they were part of a trial. He did not experience many side effects except for feeling lethargic and being less active, said his owner.
The dog had eight more treatment cycles ending in May 2022, when the tumour was found to have grown. Since then, it has shrunk slightly and has remained at 1.7cm. Oscar is now 14 and lives a normal life, with less frequent coughing and some asthma.
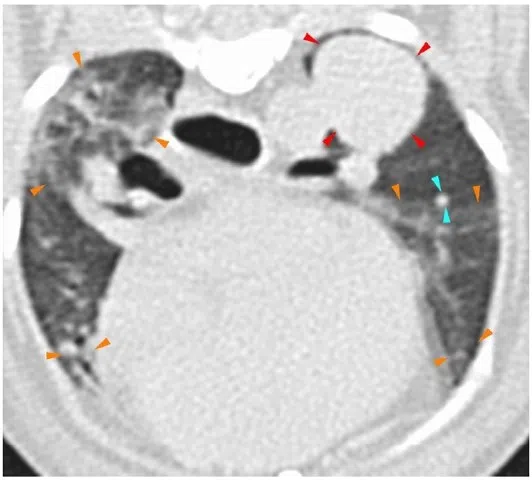
The tumour stayed at 1.7cm after Oscar underwent additional rounds of treatment.
PHOTO: NUS YONG LOO LIN SCHOOL OF MEDICINE
Dr Lee, Oscar’s vet, said: “That was one of the best outcomes we could expect from a lung tumour because it is typically quite aggressive and fast-growing.”
Ms Low, an assistant manager, added: “We are very grateful this therapy was available. If not, there would have been no other option. From a three-month prognosis, he has been living for almost three years. We’re very thankful that he is okay.”
Another poodle that benefited from the treatment was Schuyler, who had an inflamed and painful tumour in his rear that continued to grow after every surgical removal. After he underwent the novel treatment in July 2019, the tumour shrank by more than half.
And once the remaining lump was surgically removed, followed with three more therapy cycles in late 2020, the tumour never reappeared. Schuyler, who was 16, died of old age in December 2022.

Poodle Schuyler had an inflamed and painful tumour in his rear, which shrank by more than half after novel treatment in July 2019.
PHOTO: MELANIE LEE
His owner Melanie Lee, 49, said: “The treatment gave Schuyler a better quality of life. Previously, people stared and dragged their dogs away, fearing the tumour. And the oozing of blood from the tumour was unpleasant for him.”
Since 2018, the NUS Medicine team has worked out treatments using the modified stem cells for 65 sick dogs and two cats which had no other therapeutic options, as part of a trial with some local vets.
Of these, 56 lived past their original diagnosis or had a better quality of life, with 14 having tumours that disappeared for at least 30 months after treatment.
The work was published in the scientific journal BioMed Central in late 2022. Dr Ho was the first author and Dr Lee one of the co-authors.
Cancer is a top killer of dogs over 10 years old. “Cancer therapy and options for our animal patients are really far from what are available for humans. Even entire chemotherapy protocols for animals are no way as refined as those for humans,” said Dr Lee.
She noted that some pet owners are not keen to have their furry companions undergo chemotherapy, which causes side effects and affects their quality of life.
Common chemo side effects include vomiting, nausea, lethargy and loss of appetite. In severe cases, the animals could suffer from bladder inflammation, leading to blood in the urine.

Oscar is one of 56 dogs and cats with terminal cancer who either lived longer than expected, or had better quality of life.
ST PHOTO: ARIFFIN JAMAR
Dr Ho added that none of the 65 animals they treated had any serious side effects.
Dr Lee, who administered the treatment to about 10 of her canine patients, said: “This therapy provides us with the possibility that we can help our patients. Even if we don’t make them cancer-free, if we can improve their quality of life, that’s something. It gives us a little bit of hope that there is more that we can do for our patients, which is exciting.”
Now, Dr Ho and her team of five are preparing to set up a biotech start-up based in NUS Medicine which will focus on producing the therapy for both animals and humans.
The raw stem cells for animal patients are acquired from a commercial source that cultures stem cells from dogs’ fat tissues. The stem cells for human patients are sourced from a commercial cell bank, and will be further manufactured in the Health Sciences Authority’s cell therapy facility.
The team is currently able to insert the therapeutic genes into a billion stem cells each week – enough for 18 human patients.
The therapy is also expected to be more affordable and easier to scale up than existing cell and gene therapies, which commonly use viruses to carry the genes injected into the cells. The NUS team uses a chemical polymer.
Dr Ho said: “The cost of producing viral gene carriers can be between $1 million and $4 million. It could also take up to two months to produce their modified cells. For our non-viral method, the cost is less than 10 per cent in comparison, and the modified stem cells take only one week to produce, since the chemicals needed are off-the-shelf.”
The team will continue to collaborate with vets here and a veterinary professor in Hong Kong will take the therapy into animal clinical studies later in 2023.
They also plan to start clinical trials in Singapore for patients with recurrent brain cancer in 2024.


