Unique combination of operations could help save infected limbs from amputation
Sign up now: Get ST's newsletters delivered to your inbox

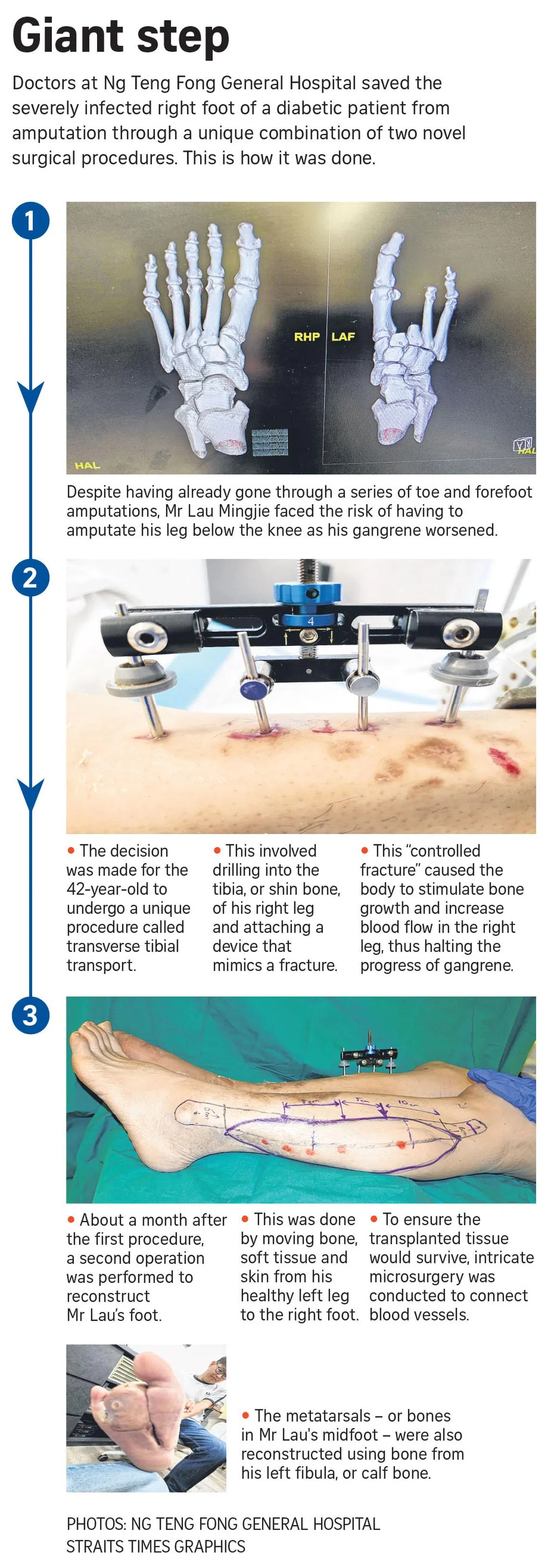
Transverse tibial transport involves drilling into the tibia, or shin bone, and attaching a small device which can mimic the effects of a fracture.
PHOTO: LIANHE ZAOBAO
Follow topic:
SINGAPORE – In May, Mr Lau Mingjie stepped on a metal nail and injured his foot. Subsequently, his foot became swollen, and he came down with a high fever and had to be admitted to Ng Teng Fong General Hospital (NTFGH).
The foot had become gangrenous – a condition where body tissue dies as a result of a lack of blood flow or bacterial infection.
As a result, the 42-year-old, who works in his family’s renovation firm, had to have the second and third toes on his right foot as well as parts of his forefoot amputated.
Despite this, the gangrene continued to progress. Mr Lau also learnt that he had Type 2 diabetes, which affects wound healing. Consequently, he faced the possibility of having his entire right leg below his knee removed.
“I couldn’t accept for it to be cut off,” he said.
It was then that Adjunct Associate Professor Chen Yongsheng, an orthopaedic trauma surgery consultant at NTFGH, presented Mr Lau with an alternative treatment called transverse tibial transport (TTT).
The procedure involves drilling into the tibia, or shin bone, and attaching a small device that can mimic the effects of a fracture.
Just as with an actual fracture, this “controlled fracture” results in stimulated bone growth and increased blood flow to the affected area, aiding recovery from the infection, Prof Chen said during a media briefing on Dec 12.
Prof Chen said that while the procedure is relatively new in Singapore, it has been performed elsewhere in recent years.
He noted that an early study on TTT by Guangxi Medical University – published in the medical journal Clinical Orthopaedics And Related Research in 2019 – showed promising results.
NTFGH became the first public hospital to perform the surgery here, as part of an emergency procedure earlier in May. It was conducted on Mr Lau later that month.
Prof Chen told reporters that not long after undergoing the surgery, Mr Lau began to show signs of improvement, with his fever going away and his foot healing.
“There was no more of the progressive gangrene that we saw with his previous four operations,” he said, adding that NTFGH has conducted eight or nine TTT procedures to date.
About six weeks after undergoing the TTT procedure, Mr Lau underwent a series of operations to reconstruct his right foot.
A team led by Adjunct Assistant Professor Vigneswaran Nallathamby – who heads NTFGH’s plastic, reconstructive and aesthetic surgery division – transferred bone, soft tissue and skin from Mr Lau’s healthy left leg to his affected right foot.
This intricate microsurgery involved connecting tiny blood vessels to ensure the transplanted tissue would survive, as well as using part of Mr Lau’s left calf bone to reconstruct his missing metatarsals, the bones in the midfoot.
This is believed to be the first time these two procedures have been combined to save a severely infected diabetic foot from major amputation, as well as reconstruct the foot to allow a patient to walk again.
Prof Chen cautioned, however, that the procedures are not a panacea for diabetic patients like Mr Lau. “I see it as yet another tool in our toolkit, in our comprehensive treatment of diabetic foot infections and severe diabetic foot infections,” he said.
He noted that as a diabetic, Mr Lau also faces the risk of future complications, such as new infections or wounds resulting from the lack of sensation in his transferred skin, which increases the risk of unnoticed injuries and subsequent infections.
“Efforts have been made to connect a sensory nerve to the flap skin in Mingjie’s case to promote sensation, and this process can take one to two years,” Prof Chen said, adding that continuous monitoring and proactive management of Mr Lau’s diabetes are essential to prevent a recurrence.
He added that Mr Lau will also require continued physical therapy to strengthen his foot and leg muscles, so as to further enhance his mobility and prevent muscle deconditioning.
Mr Lau’s recovery involved a team of healthcare professionals at NTFGH, from disciplines such as podiatry, physiotherapy and occupational therapy.
He stayed at NTFGH for four months, undergoing extensive rehabilitation to ensure he could preserve his muscle strength and walk again. Though both his feet will remain swollen from the operations for at least six to nine months, Mr Lau is now able to walk unaided, albeit with a slight limp.
He thanked Prof Chen and Prof Vigneswaran, as well as others at the hospital, for saving his leg from amputation and taking care of him throughout his stay there.
“If not, now my life will be really different. With this leg, I am able to walk again,” he said.

