MOH moves to curb rising premiums; IP riders sold from April 2026 won’t cover minimum deductibles
Sign up now: Get ST's newsletters delivered to your inbox

New riders on top of Integrated Shield Plans sold from April 2026 will no longer cover the minimum IP deductibles.
PHOTO: ST FILE
Follow topic:
SINGAPORE – To address rising insurance premiums and private healthcare costs, the Ministry of Health (MOH) is putting a stop to health insurance plans that protect policyholders almost “to the last dollar”.
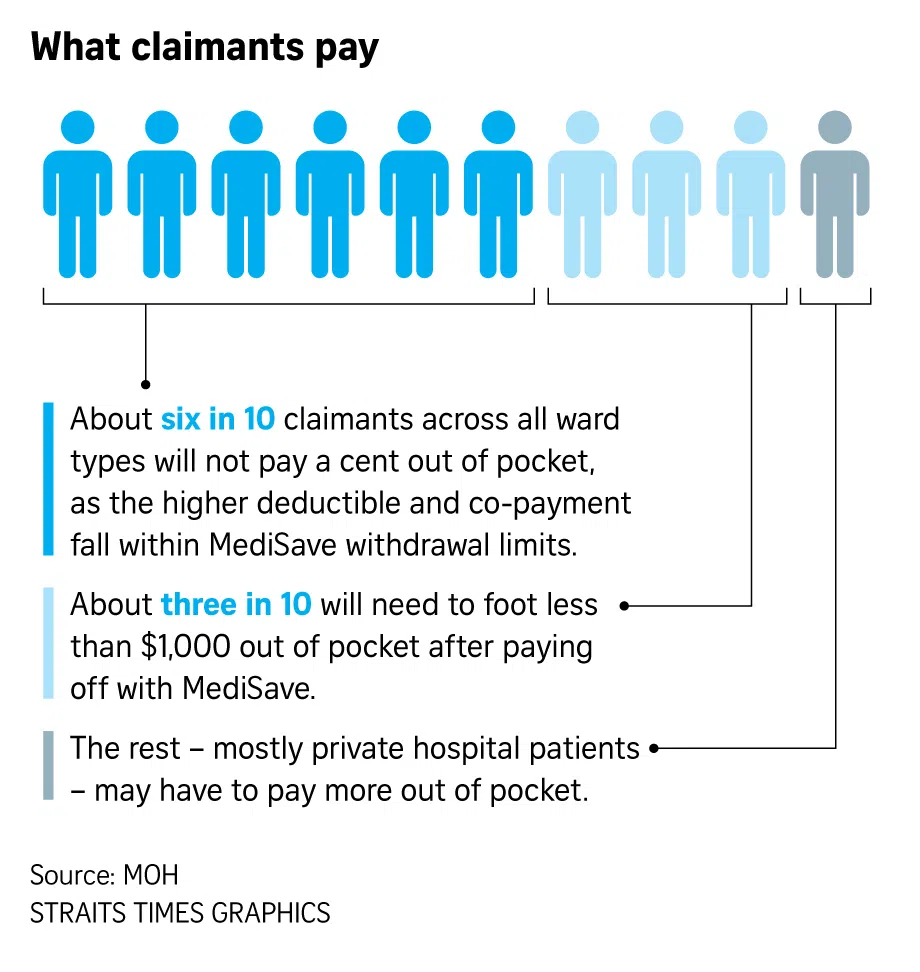
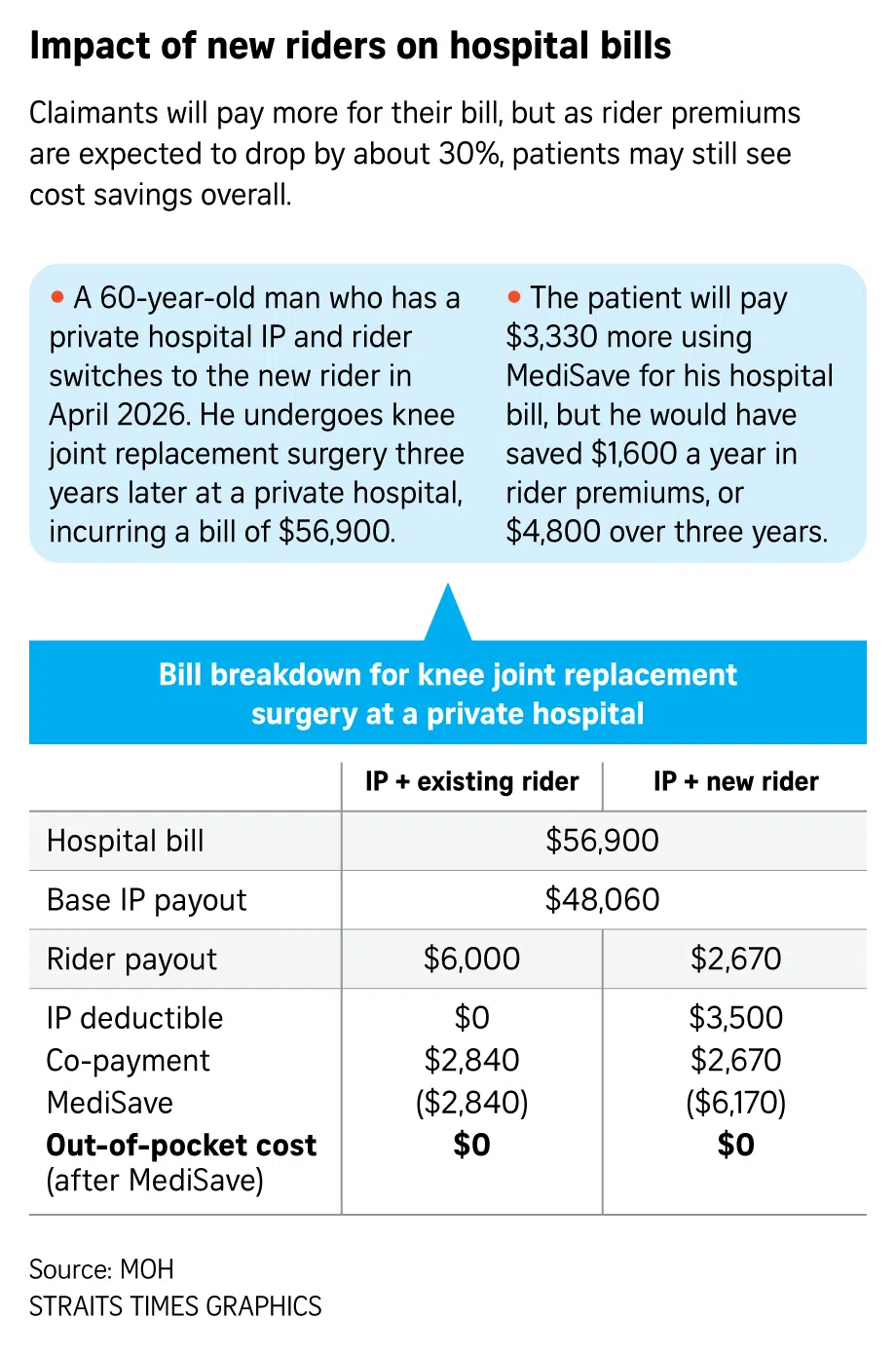
New riders sold from April 1, 2026, will no longer be allowed to cover the minimum deductibles patients have to pay before insurance kicks in. This means those with private health insurance will need to pay at least $1,500 for any hospital stay within the policy year, before they can claim from their insurer. The Integrated Shield Plan (IP) deductibles payable could go beyond $3,500.
In addition, those on the new riders will need to pay a larger portion of their bills, as the co-payment cap on their maximum out-of-pocket cash will be doubled from the current $3,000 to $6,000.
As a result, new riders are expected to cost a lot less.
MOH said it expects premiums of new riders to be about 30 per cent lower than those of existing riders with maximum coverage.
This means that Singaporeans who opt for the new riders can benefit from lower premiums while still being protected against catastrophic medical bills, the ministry said.
The new requirements will also encourage prudence, as very comprehensive coverage can be very expensive, encourage “overservicing” and drive up healthcare costs.
In terms of actual cost savings, those who choose new riders that cover private hospital stays will see average savings of about $600 on their rider premiums each year. For those choosing public hospital riders, the annual savings will be around $200.
From now until March 31, 2026, the public can still purchase existing rider products, but will have to switch to new riders that meet MOH’s requirements once the policy is due for renewal from April 1, 2028. Sales of these existing products will also cease on April 1, 2026.
As for the approximately two million Singapore residents who have already bought their riders before Nov 26, the seven IP insurers will study whether to adjust the coverage of these existing riders.
These policyholders may also wish to speak to their financial advisers and consider whether the new riders better suit their needs, MOH said.
All Singaporeans are insured under the national MediShield Life scheme, which covers expenses incurred for hospitalisation and certain outpatient treatments such as radiotherapy and kidney dialysis.
An IP is an optional health coverage provided by private insurers on top of MediShield Life, typically to cover stays in A- or B1-type wards in public or private hospitals.
On top of the IP, insurers sell riders, which are generally meant to cover the patient’s share of the bill – the deductible and the remainder of the bill not covered by MediShield Life and IPs.
On the requirement for new riders not to cover minimum deductibles, MOH said this is meant to instil discipline in healthcare consumption, particularly over minor episodes. MOH pointed out that while very comprehensive coverage that protects up to almost the last dollar can confer “absolute peace of mind” to the policyholder, it can be very expensive and can drive up healthcare costs.
With minimal cost-share, there is a greater tendency for overservicing by healthcare providers and overconsumption of healthcare services by patients.
For instance, it is commonly known that some patients choose to be warded for scans as the hospital stay is covered by insurance, even though these are “non-essential admissions”.
MOH data showed that private hospital IP policyholders with riders were 1.4 times as likely to make a claim, and that their average claim size, at $14,300, is 1.4 times that of those without riders.
Median private hospital bills have also grown from $9,100 in 2019 to $15,700 in 2024.
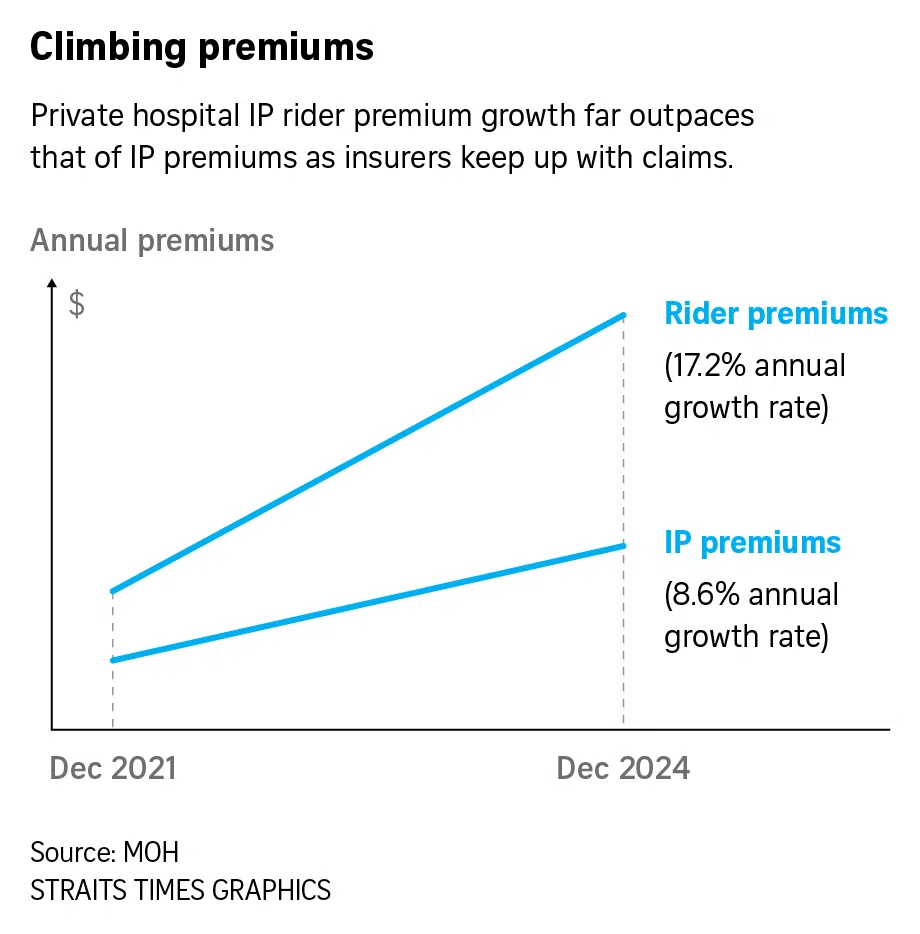
This has resulted in insurers raising premiums for private hospital IPs and riders significantly to keep up with claims, with rider premiums seeing an annual growth rate of 17.2 per cent from December 2021 to December 2024, double that of the 8.6 per cent growth rate for private hospital IP premiums over the same period.
Out of the seven IP insurers, six have increased premiums for most of their IPs or riders
Doubling of co-payment cap limits maximum out-of-pocket cash payment
The new requirements come after MOH introduced fee benchmarks in 2018 to guide pricing and guard against overcharging. It also acted on overly generous insurance designs through the introduction of rider co-payment in 2018 to rein in private sector cost escalation.
When MOH imposed a requirement of 5 per cent co-payment for all new riders sold from March 2018, IP insurers subsequently adjusted older riders
This means that after paying off the deductible, at least 5 per cent of the remaining bill still needs to be borne by the patient.
To keep pace with the increase in bill sizes over time, this cap will be doubled to $6,000 for new riders to be launched from April 2026.
While patients will pay more when they are admitted to a hospital, this will generally be offset by lower premiums each year, so they end up paying less overall. In addition, keeping premiums in check also benefits the majority of policyholders who stay out of hospitals and do not make claims.
Speaking at a media briefing on Nov 25, an MOH spokesman said that he foresees some impact of the new rider requirements on moderating overall healthcare costs to be felt almost immediately, as premiums will be lowered.
When asked about the possible impact on medical inflation, MOH cautioned against expecting any direct and immediate impact, as the issues involved are complex and will require different stakeholders to adjust their behaviours and practices.
As the new rider requirements will result in patients shouldering a higher proportion of hospital bills, MOH said it is possible that some patients with private health insurance will still opt for public healthcare.
The changes also have a longer-term objective – to set private health insurance on a more sustainable path so that it remains a viable option for Singaporeans who opt for private healthcare services, the ministry added.
The latest changes are among the various measures MOH has taken to address rising private healthcare costs. These include setting fee benchmarks to guide charging practices, taking enforcement action against doctors who make inappropriate claims, and exploring the feasibility of a new not-for-profit private hospital.
Changes fairer to policyholders as majority do not make any claims
Mr Alex Lee, president of the Singapore Actuarial Society, welcomed the changes as these will “return insurance to its original purpose of providing cover against major financial risk” and help to cultivate more mindful and efficient use of healthcare services.
He pointed out that when insurance has to pay for smaller bills, which could have been paid for with one’s personal and MediSave savings, the resulting increase in manpower and system costs to process more claims will then be priced into the premiums.
Also, buying insurance to meet smaller bills “indirectly causes policyholders to pay more in commission”, as commission is defined as a percentage of premiums.
He believes that mandating a minimum IP deductible on riders can lead to a “significant drop in IP premiums”.
Mr Lee pointed out that about 80 per cent of policyholders do not make any health insurance claims each year.
“To those who have been making efforts to stay healthy and renewing their IPs without making a claim, the latest change is fairer to them and will help reduce the cost of owning riders,” he said.
In addition, statistics show that insurers’ profit margins on private health insurance were 0.5 per cent between 2015 and 2024, which means they effectively break even, he said.
Given the competitive market, he believes that insurers are likely to continue to operate at such margins, and premiums will continue to be adjusted in tandem with changes in healthcare costs borne by the insurance risk pools.

