SGH is first in South-east Asia to perform living donor liver transplant involving incompatible blood groups
Sign up now: Get ST's newsletters delivered to your inbox
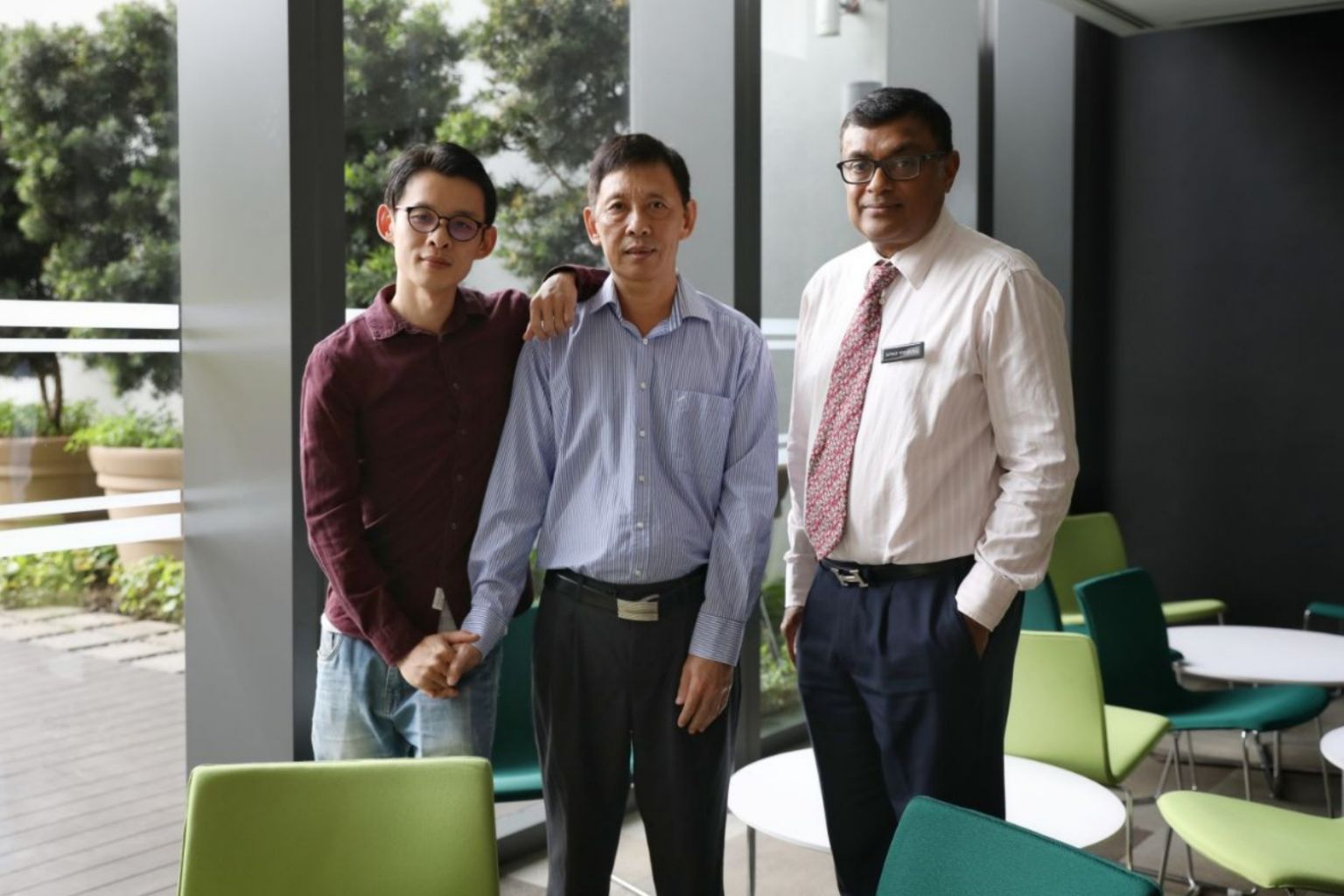
(From left) Liver donor Chen Qingzhong and his father Chen Yu Hui, together with Associate Professor Jeyaraj Prema Raj, director of the Liver Transplant Programme at Singapore General Hospital.
ST PHOTO: ONG WEE JIN
Felicia Choo
Follow topic:
SINGAPORE - A public hospital here has carried out South-east Asia's first liver transplant involving a living donor and incompatible blood groups.
In July last year, Mr Chen Yu Hui, 56 and his son Chen Qingzhong, 32, underwent a 12-hour operation at Singapore General Hospital (SGH) to replace the elder Mr Chen's liver, as he was suffering from liver cancer, hepatitis B and liver cirrhosis.
The elder Mr Chen has blood group B positive while his son has blood group A positive. Without a transplant, doctors predicted that the elder Mr Chen had fewer than two years to live.
More than a year later, father and son are both recovering well and continue to go for follow-up medical checks, SGH said in a media briefing on Thursday (Sept 20). The younger Mr Chen even had his first child - a son - born in November last year.
While kidney transplants involving living donors with blood groups incompatible with that of recipients have been performed in Singapore since 2008, this was the first such liver transplant.
Blood group incompatible organ transplants are usually a last resort, said Associate Professor Jeyaraj Prema Raj, director of the Liver Transplant Programme at SGH. "Typically, the blood group of the donor and recipient must match for liver transplant," he added.
The elder Mr Chen did not qualify for a liver from a deceased donor as such transplants are prioritised for patients with a higher chance of survival and there is concern that his liver cancer could recur, he said.
Prof Prema Raj hopes that the Chens' successful surgery will pave the way for similar surgery in the region in the future.
Such blood group incompatible liver transplants have already been carried out in places including Japan, Korea and Europe. The team at SGH studied such cases in preparation for the surgery.
Said Prof Prema Raj: "It's not something that we push; I think it's an important tool to have in certain families where there is a desperate need."
In Singapore, there is a growing number of patients on the waiting list for a liver, from nine in 2007 to 52 as of end June this year, based on statistics from the National Organ Transplant Unit.
Preparing the elder Mr Chen for the surgery involved suppressing the production of and removing specific antibodies in his blood - through an intravenous infusion and special dialysis machine - to a level low enough that would prevent them from thinking of the donated organ as a foreign body and attacking it.
Within the first two weeks after the surgery, the elder Mr Chen had to go through another round of dialysis, and the level of antibodies in his blood was measured daily to ensure that it remained low.
For the younger Mr Chen, whose wife was seven months' pregnant at the time of the surgery, the desire to save his father overrode any fear about the procedure.
Both he and his 34-year-old brother volunteered as potential donors but the younger Mr Chen was deemed more suitable.
"I felt that it was my responsibility as a son and an expression of love to help my father, so I shouldn't be too worried," said the owner of a retail shop.
After surgery, his liver took six weeks to fully grow back and he was back to work after three months.
According to a 2015 Taiwan study, the five-year survival rates for blood group incompatible and compatible living donor liver transplant recipients were similar, at 71 per cent for the first group and 71.5 per cent for the second group.

