New treatment offers hope for T-cell leukaemia that does not respond to conventional therapies
Sign up now: Get ST's newsletters delivered to your inbox

After getting an infusion of anti-CD7 CAR T-cells in December 2023, a day before her birthday, Mrs Hannah Thomas (second from right) went into remission and was discharged from NUH.
PHOTO: COURTESY OF MRS HANNAH THOMAS
SINGAPORE – Mrs Hannah Thomas’ life took an unexpected turn in March 2022 when a routine fertility test revealed she had T-cell acute lymphoblastic leukaemia, a rare type of blood cancer.
Rounds of chemotherapy and a bone marrow transplant offered the 32-year-old Australian only a brief respite. That was until an experimental treatment – CD7 CAR T-cell therapy – developed by researchers and clinicians from the National University of Singapore eventually caused her cancer to go into remission.
CAR (chimeric antigen receptor) T-cell therapy involves genetically altering T-cells – a type of white blood cells that help the body fight infections and diseases, including cancer – in a laboratory to kill cancer cells, before they are infused back into the patient.
CARs are artificial proteins which bind to specific proteins on cancer cells, helping immune cells to track down the cancer cells.
These CAR T-cells are highly effective at killing cancer cells, often within minutes. In the laboratory, they destroy 60 per cent of leukaemia cells in four hours, and 100 per cent within 24 hours.
Relating her story, Mrs Thomas, a senior policy officer at the New South Wales Ministry of Health, described how she and her then fiance, Simon, had to postpone their wedding when she suddenly found out she had cancer. It was the second postponement – the first was because of the Covid-19 pandemic.
Six months of chemotherapy and a bone marrow transplant later, she went into remission, and they eventually tied the knot in May 2023. However, their joy was short-lived, as they discovered a month later during a bone marrow biopsy that the cancer had returned.

Mrs Hannah Thomas undergoing a bone marrow biopsy in NUH.
PHOTO: COURTESY OF MRS HANNAH THOMAS
Running out of options in Australia, the couple was referred by their haematologist in St Vincent’s Hospital Sydney to the Yong Loo Lin School of Medicine at the National University of Singapore (NUS Medicine) and the National University Health System (NUHS).
They flew to Singapore in October 2023, and Mrs Thomas underwent testing for the experimental CD7 CAR T-cell therapy.
The therapy was developed by researchers and clinicians from NUS Medicine and NUHS, and had been tested on 17 patients from 2019 to 2023, including 12 at NUH and five at Ospedale Pediatrico Bambino Gesu, a paediatric hospital in Rome, Italy.
“All 17 patients have failed more than three lines of treatments – each of which can be a combination of many chemotherapy drugs – and (for the) majority of them, even bone marrow transplantation,” said Professor Allen Yeoh, who led the clinical application of this new technology.
First, T-cells were harvested from the patients. In the laboratory, the harvested T-cells were expanded and an artificial gene, known as anti-CD7 CAR, was inserted. The modified cells were then re-injected into the patient, where the anti-CD7 CAR T-cells would get to work – recognising and destroying leukaemia cells which had a protein – CD7 – on their surface, said Prof Yeoh.
This anti-CD7 CAR technology was developed by Professor Dario Campana from the department of paediatrics at NUS Medicine. He received the Singapore President’s Technology Award in 2020 for this invention.
Sixteen out of 17 patients, including Mrs Thomas, achieved complete remission within one month after treatment. Even with the use of flow cytometry tests, which can detect one leukaemia cell in 10,000 normal cells, the patients’ leukaemic cells were undetectable.
Acute lymphoblastic leukaemia – known as ALL for short – accounts for about 30 per cent of all newly diagnosed cancers in children in Singapore. T-cell acute lymphoblastic leukaemia, or T-ALL, is a rarer form of the cancer.
An estimated 85 per cent of children and 60 per cent of adults newly diagnosed with T-ALL go into remission after chemotherapy or bone marrow transplant, based on studies done in Malaysia and Singapore.
There are about five newly diagnosed cases of T-ALL that occur per year in Singapore across adults and children, said Dr Bernice Oh, the first author of the study and consultant of the paediatric haematology and oncology division in the department of paediatrics, Khoo Teck Puat – National University Children’s Medical Institute (KTP-NUCMI).
Prof Yeoh is also the head and senior consultant of the paediatric haematology and oncology division in the department of paediatrics, KTP-NUCMI and the National University Cancer Institute, Singapore (NCIS).

(From left) KTP-NUCMI’s Professor Allen Yeoh – with teammates Dr Esther Chan and Dr Bernice Oh – led the clinical application of the new CD7 CAR T-cell therapy.
ST PHOTO: ONG WEE JIN
Dr Oh added that about 80 per cent of such cases respond to conventional treatments such as chemotherapy and bone marrow transplants. The remainder that have not responded to or have relapsed after such conventional treatments will be offered the chance to undergo the new treatment.
The team’s research was published in the journal Nature Medicine on Sept 3, 2024.
After receiving an infusion of anti-CD7 CAR T-cells in December 2023, a day before her birthday, Mrs Thomas went into remission and was discharged from NUH in January before returning to Australia.
To raise funds for her treatment, their close friend, Mr Daniel Lewis, started a GoFundMe page and completed an almost 80km walk from Manly Beach to Bondi Beach in less than a day. The fund-raiser helped the couple pay for ongoing medical bills in NUH.
The amount raised was A$274,000 (S$240,000), of which more than A$100,000 came from their families and close friends.
Mrs Thomas received a second bone marrow transplant in February, this time from her younger brother, Mr Ben Langman. She has been recovering well since then and has been working from home twice a week.
A 15-year-old Vietnamese student, Viet Tai, was the first patient who underwent the therapy in 2019 when he was 10, and has been in remission for five years. He has not needed additional chemotherapy or any bone marrow transplant since.
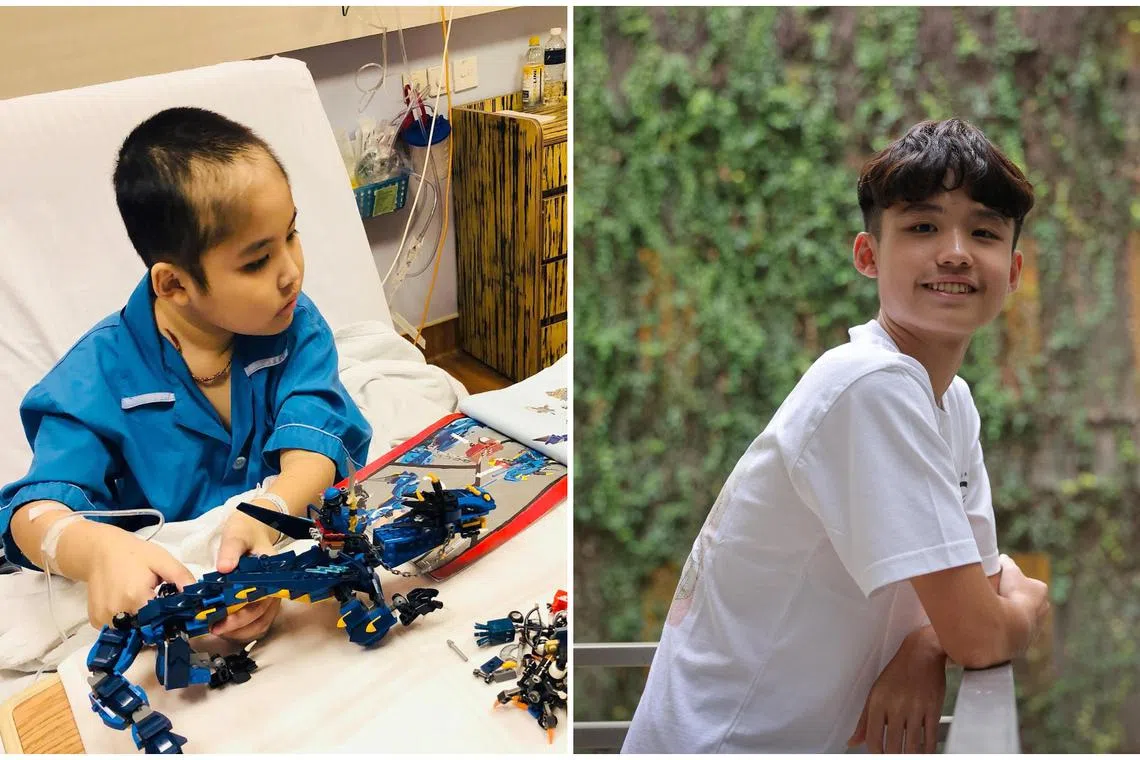
Vietnamese student, Viet Tai, now 15, was the first patient who underwent the experimental CD7 CAR T-cell therapy in 2019 when he was 10, and has been in remission for five years.
PHOTOs: COURTESY OF MADAM NGUYEN, ONG WEE JIN
“I am very grateful and thankful to all of the doctors in Prof Yeoh’s team who saved me, especially Prof Yeoh. He made the right decision, which helped me return to a normal life,” said the teenager, who wants to become a businessman so he can repay his parents for selling some of their properties and land to be able to afford the treatment.
“I also want to say thanks to all the donors and non-governmental organisations who supported me.”
Prof Yeoh said that a patient once described the ordeal of having T-ALL and receiving chemotherapy as being repeatedly hit by trains in a dark tunnel.
“With CD7 CAR T-cell therapy, we are breaking down that dark tunnel and rescuing the patient... There are no more repeated cycles of being hit by the train,” he said.
Maria Schreierer, 12, an Austrian student who suffered a relapse from T-ALL in 2022, also underwent the new treatment and stayed at NUH for four months before transferring to Vienna, Austria, for a bone marrow transplant. Prior to her treatment, her doctors in St Gallen, Switzerland, had said that her chances of survival were less than 5 per cent.

Maria Schreierer, an Austrian student who suffered a relapse from T-ALL in 2022, underwent the new CD7 CAR T-cell therapy treatment.
PHOTO: COURTESY OF MR & MRS SCHREIERER
Her parents, Mr and Mrs Schreierer, are grateful for her recovery. “We strongly believe and hope that in a few years, CD7 CAR T-cell therapy (will) become a standard therapy and not just be seen as an experimental therapy or a last chance therapy,” said Mr Schreierer.

Student Maria Schreierer (pictured in her Halloween costume) has recovered from her illness, and her father says he believes and hopes CD7 CAR T-cell therapy will become a standard type of treatment.
PHOTO: COURTESY OF MR & MRS SCHREIERER


