New hope in treating difficult triple-negative type
Sign up now: Get ST's newsletters delivered to your inbox
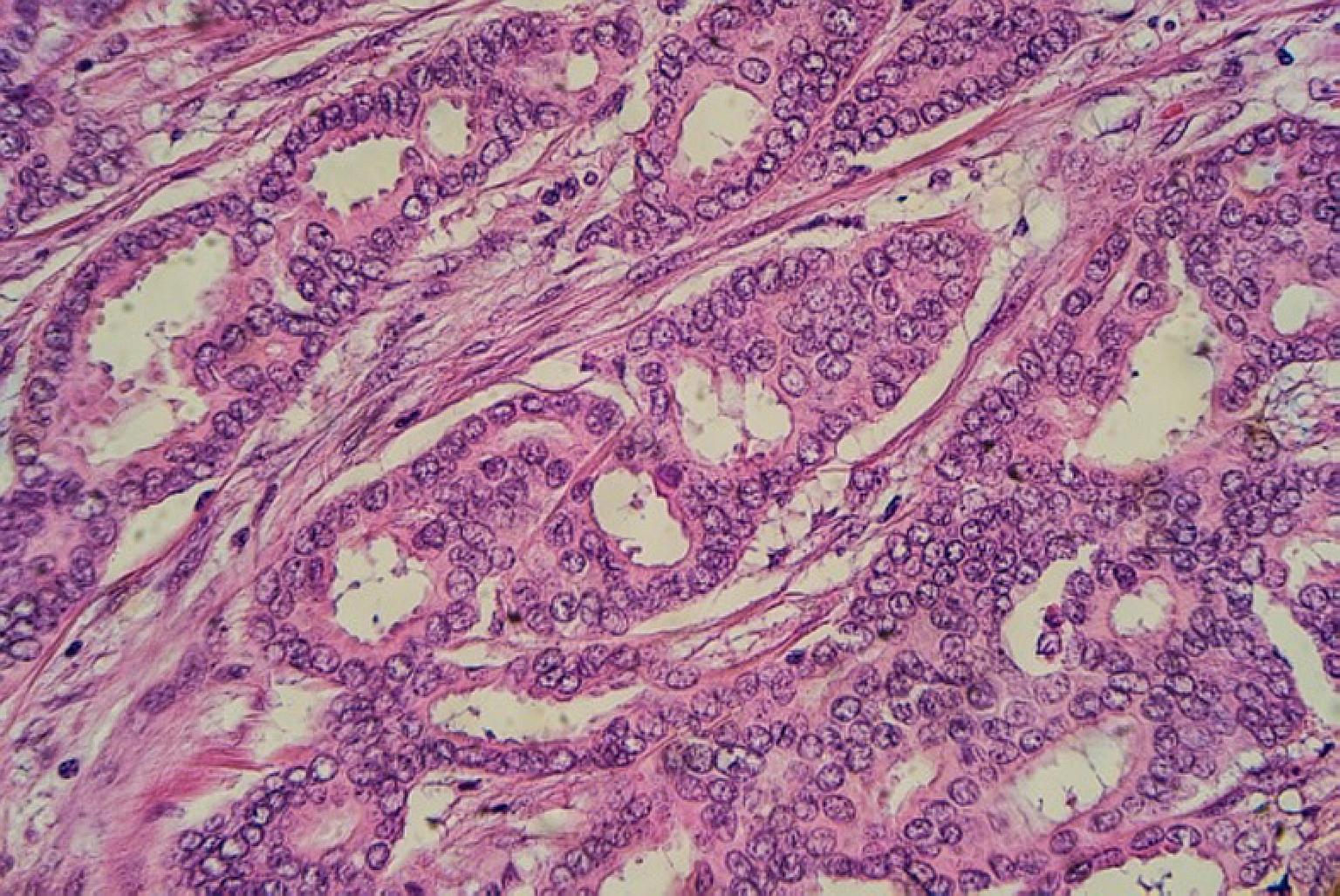
Above: Breast cancer cells. Around 1,900 women were diagnosed with breast cancer yearly from 2010 to 2014.
PHOTO: A*STAR
Survival rates for breast cancer have never been higher, but one form of the disease still evades the arsenal of scientists and doctors - triple-negative breast cancer (TNBC).
This type of cancer afflicts around 10 per cent of around 1,900 breast cancer patients here yearly but lacks targeted treatment.
Its growth is neither supported by the hormones oestrogen and progesterone, nor by the presence of the human epidermal growth factor receptor 2 (HER2) protein, which regulates the growth and spread of breast cancer cells, and has been known to cause the cancer to be more invasive and aggressive.
It therefore does not respond to hormonal therapy such as tamoxifen or aromatase inhibitors, or treatments that target HER2 receptors, which have worked well against other forms of breast cancer.
But there is hope.
Working together, oncologists at the National University Cancer Institute, Singapore (NCIS) and the National University of Singapore's (NUS) Yong Loo Lin School of Medicine have found two novel drug combinations that could potentially treat TNBC. They are existing forms of medication that are being used to treat other conditions, such as ovarian cancer and a rare type of lymphoma, but not breast cancer.
"As these are available drugs, if we are able to get through negotiations (with drug companies), it is possible we can have the trial in 12 to 18 months," said Associate Professor Lee Soo Chin, who will lead the study.
Prof Phillip Koeffler of the NUS Cancer Science Institute of Singapore, who is also deputy director (research) at NCIS, tested the combinations in cancer cells in the lab and found them to be effective. The plan is to move on to animal tests.
In another promising development, scientists from the Agency for Science, Technology and Research's Genome Institute of Singapore (GIS) and the Cancer Science Institute of Singapore (CSI) have found a new way in which the EZH2 gene activated in numerous cancers promotes the growth of breast cancer, especially in TNBC.
EZH2 - which plays a role in cell development - has long been known to impair the body's ability to stop the growth of cancer tumours, when mutated or over-expressed.
Now, the scientists have found that when the tumour cells are starved of oxygen, EZH2 engages another well-known tumour-promoting gene, FoxM1, to promote breast cancer invasion.
The finding was published in journal PNAS in June.
"Interestingly, this phenomenon seems to be more common in TNBC, as compared to other types of breast cancer," said GIS Professor Qiang Yu who co-authored the study.
He added: "Now that we have identified a new pathway of EZH2 in promoting TNBC invasion, this finding may lead to a new treatment strategy to target TNBC, a disease in which effective treatments are currently lacking."
Overall, scientists and doctors are still trying to make sense of what drives different breast cancers to progress or relapse.
Some 1,900 women were diagnosed with breast cancer in Singapore each year between 2010 and 2014. A total of 2,051 died from it over that period.
In a clinical trial at NCIS, the body's natural killer cells are being used to stop late-stage breast cancer from progressing - a world first.
One of the latest efforts comes from the Yong Loo Lin School of Medicine, which is approaching the battle from several fronts, boosted by $1 million in funding from the NCIS Yong Siew Yoon Research Grant for translational research.
Apart from searching for drug combinations to treat TNBC, the team will start two very preliminary studies looking at chemicals that work to block two specific proteins secreted by cancer tumours, which cause them to spread and become resistant to treatment.
Due to the studies' early stages, It will take at least three years for them to get to clinical trials, said Prof Lee.
Another path to understanding cancer is being explored by Associate Professor Mikael Hartman from the NUS Saw Swee Hock School of Public Health. He has led the Singapore Breast Cancer Cohort study for the last five years, collecting data from patients such as their lifestyle habits and other illnesses they may have at the same time.
He has had 6,000 participants so far, and estimates another 5,000 will take part in the next three years.
"We can compare the genetic make-up of these women with healthy women, which will allow us to better understand the genetic background to breast cancer," said Prof Hartman.
Researchers can also look within the cohort to find women who would benefit most from certain treatments, or identify groups of patients who are receiving incomplete treatment options, he added.
So far, Prof Hartman and his team have isolated close to 70 genetic markers for breast cancer, which could help to predict how likely a woman is likely to develop cancer.
"The overall goal is to find out who will develop cancer, how to detect it early, find out how we treat different types of the cancer, and to improve quality of life after treatment," he said.
Find out more about cancer and how to fight it on ST's Fighting Cancer microsite.


