More patients receive hospital-level care at home with expansion of MOH programme
Sign up now: Get ST's newsletters delivered to your inbox

NUH patient Paul Faulkner with NUHS@Home nurse clinician Claudia Tan (left) and NUHS@Home lead Stephanie Ko.
ST PHOTO: KELVIN CHNG
Follow topic:
SINGAPORE – More patients have been receiving hospital-level care in their homes as the nationwide Mobile Inpatient Care @ Home programme (MIC@Home) is progressively expanded to those who had not been admitted into hospitals.
These patients include those who were referred to the programme through private general practitioners (GPs), polyclinics, community care teams and nursing homes.
When the Ministry of Health (MOH) officially launched MIC@Home in 2022 after earlier pilots, the programme was for patients who were recovering after hospital stays, to ease the demand for hospital beds.
On Oct 3, the National University Health System (NUHS) announced that its version of the programme, called NUHS@Home, has cared for nearly 7,000 patients at home to date, and saved over 42,000 hospital bed days.
NUHS, a public healthcare cluster looking after the population in the west, piloted NUHS@Home in September 2020.
At the fifth anniversary celebrations of NUHS@Home, the cluster said it has progressively expanded the programme since 2024.
Up till Aug 31, it had cared for about 200 patients referred through community touchpoints – 56 by NTUC Health’s nursing homes, 64 by NUHS’ community care teams, and the rest by polyclinics or GPs.
These patients had conditions such as pneumonia, urinary tract infections and cellulitis, which commonly affect older adults with limited mobility.
They would otherwise have had to be admitted to an acute hospital, adding to the demand for hospital beds.
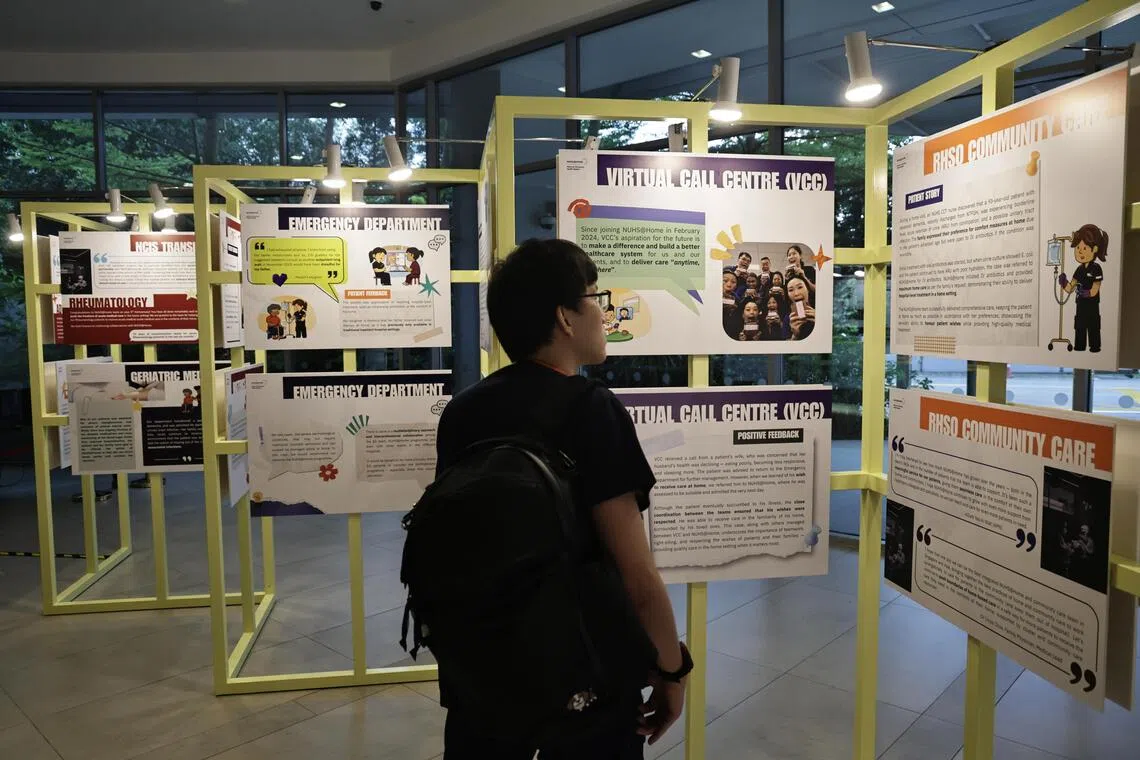
A NUH staff member viewing an exhibition at the fifth anniversary celebration of NUHS@Home on Oct 3.
ST PHOTO: KELVIN CHNG
Apart from NUHS, the other two public healthcare clusters in Singapore have also implemented the home care programme.
SingHealth, which takes care of the population in the east, similarly provides home-based care to patients who were not admitted to its hospitals, and is working on extending services to more patients.
Professor Lee Chien Earn, deputy group chief executive officer of SingHealth, told The Straits Times the cluster has been accepting referrals for home-based care from its polyclinics for neonatal jaundice cases since January 2024.
Sengkang General Hospital (SKH), which is part of SingHealth’s cluster, has also been trialling its SKH@Home service with Grace Lodge Nursing Home residents since October 2023.
Associate Professor Toh Hong Chuen, clinical lead for NHG Health’s MIC@Home programme, said the cluster is planning to expand the service to patients referred through the community, as well as to patients whose psychiatric conditions are assessed to be suitable for home-based care.
NHG Health takes care of the population in the central and north regions.
Under MIC@Home, patients are cared for by teams of hospital doctors, nurses and allied health professionals in the comfort of their own homes through a combination of teleconsultations and home visits.
Mr Paul Faulkner, 65, first heard about the home-based care programme in 2024 when he was recovering at the National University Hospital (NUH) after undergoing open-heart surgery.
Following a two-month stay at the hospital, he felt that he was recovering well, although he needed intravenous injections of antibiotics. So, he discussed with the NUH doctors if he could be discharged and continue to be cared for at home instead.
After the care team assessed that his living environment was suitable, and as his wife was available to be his caregiver, he was given a thorough briefing, which included advice on how to monitor his condition at home, before being transferred to the NUHS@Home programme.
Mr Faulkner appreciated the efforts made in allowing patients in stable condition to return home earlier, including daily calls from the care team to check on his condition, and home visits once every two days for antibiotics administration.
“It was certainly a relief and positive step forward... after having been in the hospital for so long, you are actually back at home, being looked after and definitely recovering,” he said.
NUHS@Home offers 100 virtual ward beds and is currently run by 160 staff. NUHS plans to expand the programme to 400 beds by 2030, with a vision of making home-based care a default model of care for patients, with patients warded only if there is really a need.
Patients who opt for MIC@Home are supported by subsidies, MediShield Life, MediSave and Integrated Shield Plan coverage.
Based on NUHS information, a subsidised patient transferred from a Class B2 ward to the NUHS@Home programme will pay $43 each day, compared with a daily fee of $57 in an NUH general ward.
The daily charges for a Class C ward patient would be $39 for NUHS@Home and $52.40 in a general ward in NUH.
Patients who are directly transferred from the hospital’s emergency department or via community referrals are considered Class C ward patients by default.
These figures assume a patient receives the maximum government subsidies, and do not include daily treatment fees and other fees such as those for medication and laboratory tests.
NUHS@Home charges are slightly lower than inpatient ward charges, and the charges for home-based care patients include services, such as home visits and delivery of medication.
At the NUHS event, Professor Kenneth Mak, MOH’s director-general of health, thanked the patients and family members who have trusted the home-based care programme, and healthcare staff and partners who support the programme.
With MIC@Home set to expand further to benefit more patients, “patient safety, clinical governance and quality of care remain absolute priorities and important to us”, said Prof Mak.
Correction note: In an earlier version of the story, we said that while NUHS@Home charges are slightly lower than ward charges, home-based care patients have to pay for other services, such as home visits and delivery of medication. NUHS has clarified these are not additional charges and are part of the NUHS@Home charges.

MOH’s director-general of health Kenneth Mak speaking at the event on Oct 3.
ST PHOTO: KELVIN CHNG

