Local researchers are one step closer to creating a safer and faster method to grow human skin for skin grafts for burns patients.
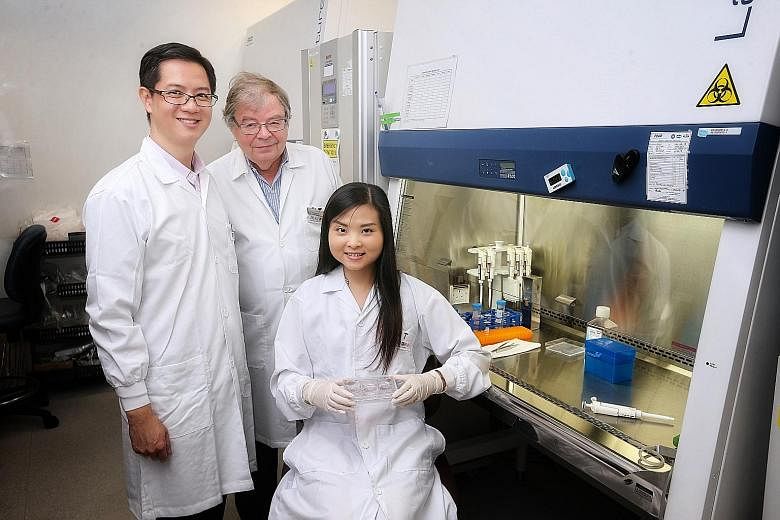
In this new method, which is the first in the world, a human protein called laminin is combined with human skin cells in the laboratory to grow new skin, researchers from Duke-NUS Medical School and Singapore General Hospital (SGH) said on Thursday.
Laminin binds cells together in the body.
As the protein comes from humans, it would likely not pose any risk of infections or adverse immune reactions in patients, unlike the current 40-year-old method of combining mouse cells with human skin cells to grow new skin, said Professor Karl Tryggvason from Duke-NUS Medical School's Cardiovascular and Metabolic Disorders Programme.
Animal-derived products and biological agents used in the process of cultivating skin cells are considered high-risk under a pharmaceutical standard called the Good Manufacturing Practice system.
Regulatory agencies such as the US Food and Drug Administration have classified such cultured products as xenografts, which are approved only for treatment of severe burns that cover more than 30 per cent of the total body surface area.
-
200
-
Average number of burns patients seen by SGH each year - 10 per cent to 15 per cent of them have severe burns which need to be treated with cultured skin grafts grown from their own skin cells.
The new method, which uses laminin proteins LN-511 or LN-421, is also faster at growing new skin than the current method, said Dr Alvin Chua, deputy head of the Skin Bank Unit at SGH's Department of Plastic, Reconstructive and Aesthetic Surgery.
This means that patients could get skin grafts faster, which would speed up their recovery and shorten their hospital stay, added Dr Chua.
The process of growing skin with laminin, which is produced in the laboratory, takes three to four weeks, which is up to a week faster than using mouse cells, he said.
SGH sees an average of 200 burns patients each year, and 10 per cent to 15 per cent of them have severe burns which need to be treated with cultured skin grafts grown from their own skin cells.
So far, the new method has been shown to grow new skin as effectively as the older method when tested on mice, said Prof Tryggvason.
The study, conducted from February 2014 to last month, was published in the journal Nature Communications last month.
The next step is to embark on a clinical trial in mid-2019 involving around 10 patients from SGH to test its effectiveness on humans, added Prof Tryggvason, who is also the lead author of the study.
If successful, the new method could potentially be used to treat any kind of burns and other skin defects like chronic wounds, said Dr Chua, who is also an adjunct assistant professor of Duke-NUS Medical School's Musculoskeletal Sciences Academic Clinical Programme.
Researchers are hopeful that the new method will replace the older one in about five years' time.