Healthcare clusters focus on building community support as Healthier SG roll-out draws near
Sign up now: Get ST's newsletters delivered to your inbox
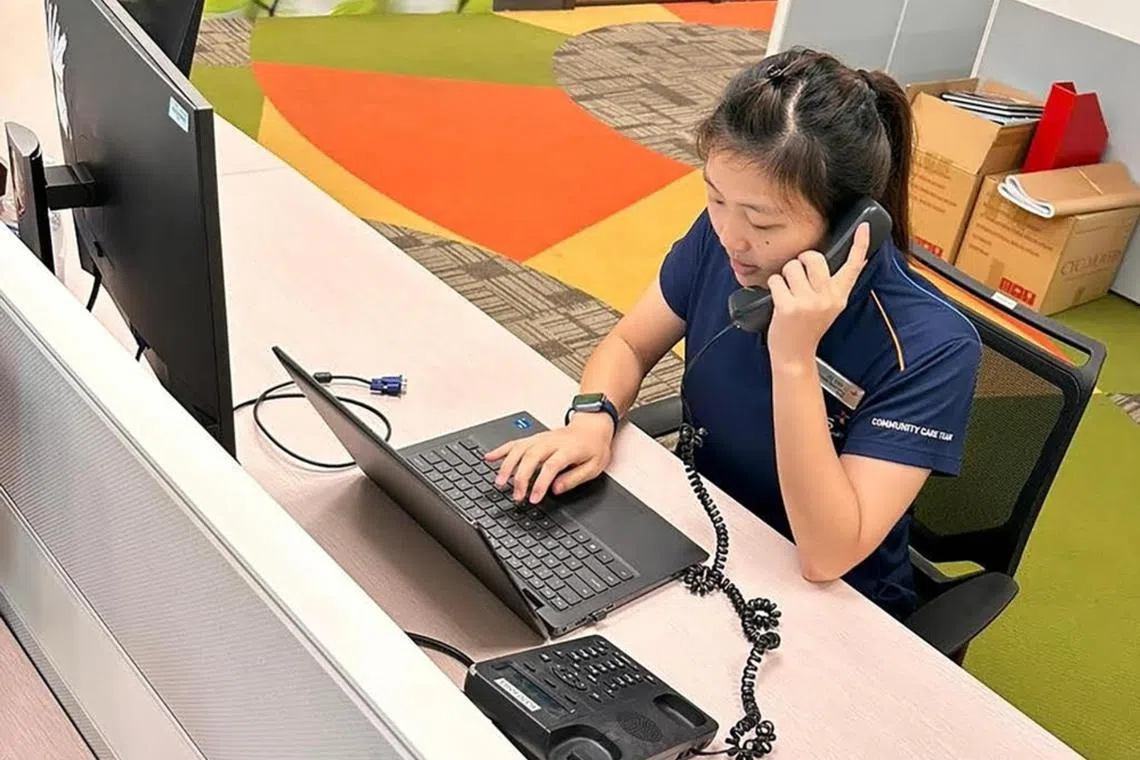
Care coordinators can support the GPs with some of the Healthier SG work.
PHOTO: NUHS RHSO
Follow topic:
SINGAPORE – The preparatory work at the three healthcare clusters has intensified as the roll-out of Healthier SG, Singapore’s major preventive care strategy, draws near.
The work includes engaging general practitioners (GPs), offering them training on team-based approaches, and growing the teams of community nurses and coordinators to support residents.
Healthier SG aims to shift the centre of gravity in healthcare
The National Healthcare Group (NHG), Singapore Health Services (SingHealth) and the National University Health System (NUHS) will shift to focus on primary and community care.
They are working with the Ministry of Health and the Agency for Integrated Care to engage and recruit GPs for Healthier SG, as they continue to strengthen the community support for residents and GPs.
To prepare GPs for Healthier SG, the Primary Care Academy, run by NHG Polyclinics (NHGP), has developed a primer for them, said its director, Dr Irwin Chung.
It consists of workshops and online training on topics such as preventive care and behavioural counselling, as well as workshops for clinic assistants.
The training is team-based, because from what has been learnt in the polyclinics, primary care should slowly evolve into a non-doctor-centric outfit, he added.
Dr Darren Seah, director of family medicine development at NHGP, said this is possible because GPs need to be part of a network supported by nurses and care coordinators – known as a primary care network (PCN) – to come on board Healthier SG.
The PCN scheme was piloted in 2012 to improve chronic disease management in the community.
In December 2022, Health Minister Ong Ye Kung said half of the GP clinics here – or 800 clinics – have joined PCNs,
Dr Seah said some PCNs have reinforced their set-ups with nurses and allied health professionals.
“That’s what we see internationally as well... (For instance) I’m not the best person to give dietary advice, it tends to be really standard. A dietitian can do a lot more,” he added.
Dr Seah is also the scientific committee organising chairman of the first Singapore Primary Care Conference, which will be held on March 3 and 4.
He said the event will address some of the new challenges in primary care as the role of GPs continues to evolve, particularly with Healthier SG, when GPs will take on more of the chronic disease management work that has traditionally been the domain of polyclinics.
“(GPs and polyclinics) will enrol patients, and there are some similarities to the work that we do in the future, so it’s probably a good time to break down whatever silos that have existed before and come together as a community,” he said.
At SingHealth, teams of community nurses, well-being coordinators, primary care providers and community partners are being developed. They will be sited in more than 30 areas in the eastern part of Singapore, said Professor Lee Chien Earn, its deputy group chief executive (regional health system).
“Our aim is to co-develop personalised care plans taking into account (patients’) life stage, and health and social needs,” he added.
In the western region, NUHS has engaged GPs over the years and works with more than 130 of them. The plan is to add more community health posts, which are manned by community nurses and primary care coordinators who will work closely with GPs and community partners, said Ms Joanne Yap, executive director of its regional health system office.
There are already more than 30 of these posts, where residents can go to find out about the health services nearest to their home, she added.
In the central north region, NHG said community health teams comprising nurses, allied health professionals and health coaches will work alongside GPs and community partners.
Dr Chung said that at the start of Healthier SG, there is a good chance that most of the people who enrol with GPs are those who are already seeing the GPs for their chronic conditions.
The care they get, however, may be more specific. For instance, if a patient with hypertension is smoking, his GP may ask him to quit the habit.
“But with Healthier SG, you should be referring this patient to a smoking cessation programme,” he added.


