askST: What should I know about the new riders of MediShield-linked Integrated Shield Plans?
Sign up now: Get ST's newsletters delivered to your inbox

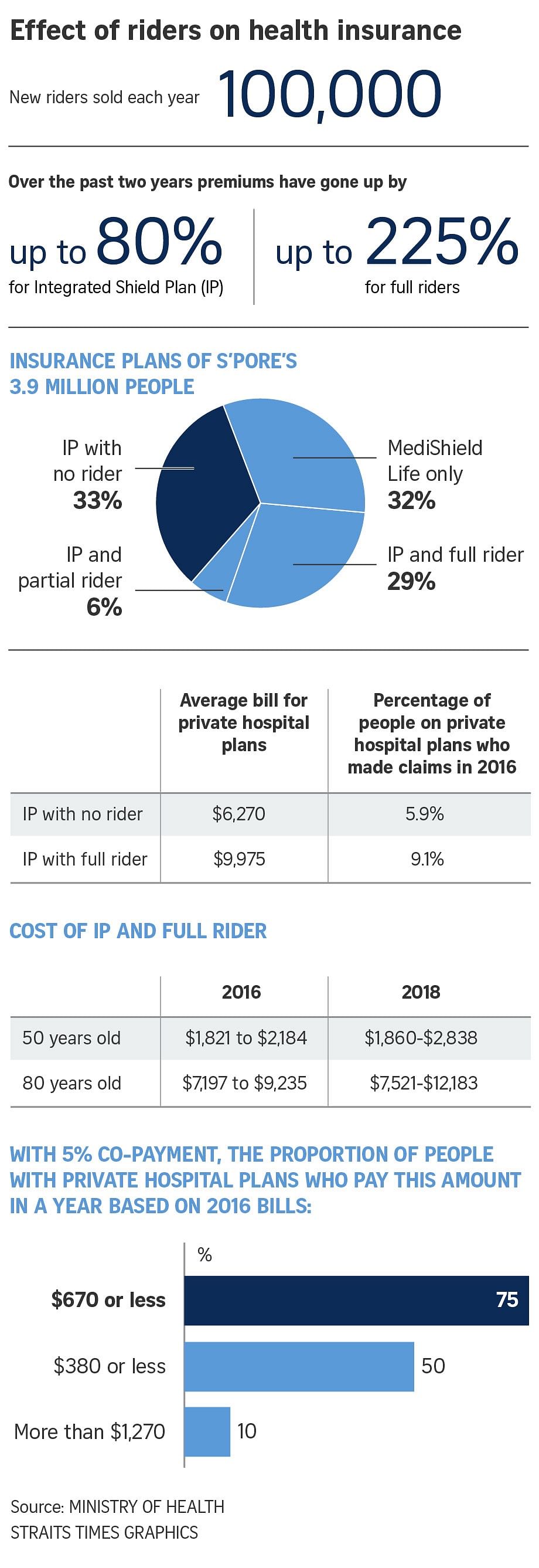
All riders sold from March 8 must, eventually, have a co-payment element of at least 5 per cent of the hospital bill.
PHOTO: ST FILE
SINGAPORE - On Wednesday (March 7), the Ministry of Health (MOH) issued requirements for new riders of Medishield-linked Integrated Shield Plans (IPs).
All riders sold from March 8 must, eventually, have a co-payment element of at least 5 per cent of the hospital bill. But the total amount that a policyholder has to pay can be capped at $3,000 a year.
The cap is contingent on two things: policyholders are treated by doctors on the insurer's panel; or they have had pre-authorisation from the insurer to seek treatment from doctors not on the panel.
If these are not met, the policyholder will need to pay 5 per cent of their bills, with no limit on how much they need to pay each year.
askST finds out answers to some commonly asked questions on this issue.
Q: Which insurers have panels of doctors?
A: Currently, four of the six IP insurers do, namely AIA, Aviva, AXA and Great Eastern. Some of the panels are still small and being built up.
NTUC Income and Prudential will have to come up with doctor panels in the coming year if they want to offer caps to what holders of their new rider policy need to pay annually. Income says it is working on this.
Q: Why do insurers want people to go to doctors on its panel?
A: Prices charged by doctors in the private sector for the same treatment can vary widely, even if the outcome is the same. This is because doctors are free to charge what they want.
Insurers - and also the Health Ministry - want to encourage policyholders to seek treatment with doctors whose charges are more reasonable.
For some insurers, like AIA, all public sector doctors are treated as approved doctors on its panel.
Q: How do insurers chose their panels?
A: Insurers say doctors are invited to join their panels based on the insurers' claim experience over the years.
These would be doctors whose fees are considered reasonable by the insurer, who are preferred by policyholders, and who have no "black marks" against them, such as complaints of poor service.
A doctor can be on the panel of more than one insurer.
Q: Do these doctors get any payment from the insurer?
A: No, such payments would be considered kick-backs and disallowed. Doctors are also not allowed to pay insurers to channel business their way.
Q: Do policyholders get better rates or discounts when they use doctors on the panels?
A: That would depend on the agreement of the insurer and the doctor. AXA and Great Eastern, for example, have pre-negotiated rates with the doctors on its panel.
Q: How do I know who is on my insurer's panel?
A: Some insurers have hotlines, others provide a list of doctors. Policyholders can also check with their agents.
Q: What is the process of being seen by a doctor on the panel? Is a letter required from the insurer or a GP?
A: No letter is required. But some insurers require patients to check on the treatment before giving approval. You can also make an appointment to see the doctor, who will liaise with the insurer. There is unlikely to be a dispute on the bill. The 5 per cent of the bill the holder need to pay him will be counted towards the $3,000 annual cap.
Q: What happens if the policyholder does not want to see a doctor from the panel? Can he go ahead or must he get a waiver from the insurer?
A: The policyholder could approach the insurer to authorise the treatment. If the insurer authorises it, the insurer will pay the bill and the 5 per cent co-payment by the policyholder will count towards the latter's annual $3,000 cap.
AXA says it takes three hours to evaluate requests in an emergency, and three days in non-urgent cases. Great Eastern also takes about three days but only pre-authorises treatments if done by doctors on its panel. Aviva says it needs five days.
Should the policyholder not apply to the insurer for pre-authorisation, or should the insurer deny the request, the policyholder can still be treated by the doctor. But there will be no cap on the 5 per cent share of the bill.
Q: What happens if it is an emergency and the doctor treating the policyholder is not on the panel, and there was no time to get pre-authorisation?
A: A spokesman for the MOH said insurers should not disadvantage policy holders in the event that they have to seek treatments from non-panel doctors or without pre-authorisation because of a genuine emergency. Insurers should take this into account as they design and implement panels and pre-authorisation processes.
An AIA spokesman said that if its policyholders are taken by SCDF ambulances to a public hospital, it would not be a problem since all public sector doctors are "approved". Should the policyholder go to a private hospital, he could ask to be treated by an AIA-approved doctor. In such cases, the patient's portion of the bill will be capped.
Q: What does it mean to have "pre-treatment approval" from the insurer? And how does a patient get this?
A: This varies with insurers.
Some require the policyholders to call a hotline, or fill up a form, to seek approval. In some cases, a letter of guarantee is provided by the insurer upon approval. For some, pre-approval for treatment is needed even when seeing a doctor who is on its panel. For others, it is only if the doctor is not on its panel.
Q: How can a policyholder be assured he won't be under-treated by a doctor on an insurer's panel?
A: This is unlikely to happen as there is no reason for a doctor to do that. The doctor is not employed by the insurer. He is merely "approved" by it.
Dr Leow Yung Khee, Group Medical Director of Great Eastern said: "The doctors are given full autonomy in their clinical judgement and decisions."

If the doctor under-treats, patients would need further treatment, and this might end up more costly for the insurer.
Doctors might want to keep their bills "reasonable" to remain on the insurer's panel, as this would likely generate more business for them.
But Professor Teo Yik Ying, Dean of the Saw Swee Hock School of Public Health, said: "The provision of fewer services in itself is not wrong, as long as that level is exactly what is required to treat the patient.
"I believe there are enough guidelines in place that panel doctors will be prudent and careful with providing the treatment necessary to address the conditions. It is unlikely that doctors will risk their professional licences just to save money for the insurers."


