Covid-19 chaos at China’s hospitals as stringent control policy eases
Sign up now: Get insights on Asia's fast-moving developments
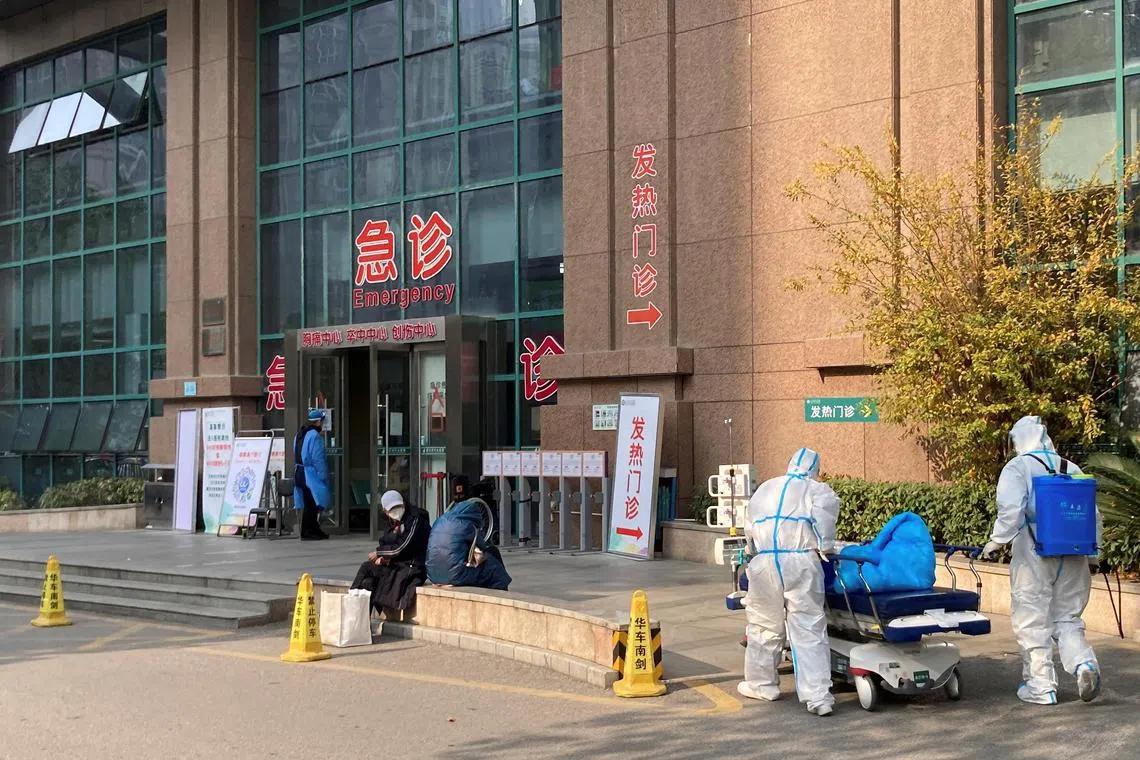
For health-care workers at hospital emergency rooms, one of the challenges is separating Covid patients from non-Covid cases.
PHOTO: REUTERS
BEIJING ( CAIXIN GLOBAL ease the burdens of sweeping pandemic lockdowns,
Since the State Council, China’s cabinet, rolled out a new 10-point plan Wednesday to ease its stringent Covid-19 controls, ending mass nucleic acid testing and allowing some infected people to quarantine at home rather than in centralised facilities, hospitals are facing increasing workloads as infections surge.
In cities such as Guangzhou, Shijiazhuang and Beijing that have taken the lead in implementing the new policy, fever clinics are full of patients and cross-infections
Experts predict a peak of infections in the next one to three months with about 60 per cent of the population infected, which would squeeze already swamped hospital emergency rooms and intensive care units and burn out health-care workers.
Faced with difficulties such as the shortage of intensive care resources, a significant urban-rural gap in health resources and still-immature telemedicine, mitigating the impact of the coming surge has become the biggest challenge facing China as it continues the shift from the stringent “zero-Covid” strategy.
Overwhelmed hospitals
In some cities, the first shock wave has already hit.
In the central city of Wuhan, the epicenter of China’s Covid-19 outbreak in early 2020, the authorities published a list Dec 1 of 42 fever clinics, but some of them closed only a couple of days later because of too many infected patients and staff.
For health-care workers at hospital emergency rooms and fever clinics, one of the challenges is separating Covid patients from non-Covid cases. “Some patients came to the hospital with normal temperature after taking fever medicine but tested positive later, causing cross-infection at the hospital,” said Shao Yang, an ER doctor in a Wuhan hospital.
According to the ninth version of Covid-19 diagnosis and treatment guidelines issued by the National Health Commission in March, hospitals are required to treat patients with suspected cases in single rooms while waiting for nucleic acid test results and to place confirmed infected patients under centralized quarantine or send them to designated hospitals.
But in reality, such measures can’t keep up with the surging number of infections. A doctor at a Beijing hospital said about 20 per cent of the hospital’s doctors were off duty due to their own infections or close contact with infected patients, leaving the rest of staff a heavier workload. A doctor at a Guangzhou hospital said the hospital is severely understaffed as more than 200 people have been dispatched to makeshift quarantine hospitals.
When a patient is found to be infected, hospital staff members need to get tested, the ward needs to be sterilized and some surgeries and special treatments have to be canceled.
The grandson of a lung cancer patient in Beijing said his grandfather was scheduled to receive chemotherapy Nov 25 at Beijing Cancer Hospital, but positive patients were found in some wards and the whole hospital was closed, placing his grandfather’s treatment on hold.

People line up at a fever clinic of a hospital in Wuhan on Dec 10, 2022.
PHOTO: REUTERS
Many hospitals in Beijing have suspended receiving cancer patients, said the grandson, who volunteers at a cancer patient help group. The group found that thousands of cancer patients were recently unable to receive chemotherapy.
A nephritis patient in the northeastern city of Ha’erbin said he needs dialysis every other day, but now he hasn’t received the treatment for six days. Almost all the nurses in the dialysis department are under quarantine as positive Covid cases were found, he said.
Shortage of medical resources
What’s even more worrying is the threat of severe cases, which usually come after the peak of total cases, spreading the stress from fever clinics to intensive care units.
The vast majority of Covid patients have mild symptoms, but given the huge totals, there may still be a high number of severe cases, resulting in a shortage of medical resources,
When a big outbreak of the highly contagious Omicron variant early this year caused nearly 6,000 deaths in Hong Kong, a large number of residents who tested positive flooded into emergency rooms of public hospitals, resulting in severe overcrowding. Now the Chinese mainland faces a similar challenge.
Under the previous Covid control model, community workers and grassroots pandemic prevention personnel undertook the main work of detection, transfer and isolation of infected people. But under the new guidelines, hospitals are the first line of defence.
It has been a common practice for hospitals to require a negative nucleic acid test result within the previous 24 hours to enter the hospital. In a notice issued Thursday, the State Council made clear that any residents, regardless of whether they had nucleic acid tests or what the results were, can visit fever clinics, and hospitals should make sure fever clinics are open 24 hours a day.
After the removal of the testing requirement, hospitals immediately felt the pressure. When Caixin reporters called a score of hospitals in Beijing and Wuhan on Dec 6, several of them said their outpatient clinics were temporarily closed after receiving positive patients.

The vast majority of Covid patients have mild symptoms, but given the huge totals, there may still be a high number of severe cases.
PHOTO: REUTERS
Under the overwhelming pressure, some hospitals have brought back the previous requirement of negative nucleic acid test results for patients. Some even require that patients wear N95 protective masks throughout visits.
Another difficulty plaguing hospitals is how to separate Covid patients and non-Covid patients, which puts greater demands on manpower, resources and facilities.
Guangzhou Women and Children Medical Center recently expanded its fever clinics from 2,100 square meters to 2,600 square meters and from seven exam room to 13. It also set up zones for negative, positive and pending-result patients. Staff working in each zone are required to reduce contact with other areas.
However, in reality, when swamped with large numbers of patients with fevers, many hospitals with limited resources are essentially not implementing zoning arrangements. A staff member at a major Guangzhou hospital told Caixin that all the hospital can do now is to have the staff tested every day to ensure no positive workers are on duty.
Several hospitals also mentioned that a number of medical staffers were dispatched to support makeshift quarantine centers and that they had to reduce the number of beds in use due to a shortage of nurses.
Ensure no interruption
Under the State Council’s 10-point plan, authorities made clear that if medical workers test positive, close contacts should be accurately identified, but hospitals should not be locked down to ensure normal medical services.
But identifying close contacts and avoiding service interruptions is a fine line to walk. A doctor at a large hospital in Beijing said that staff members may not be considered close contacts if they wear N95 masks while coming into contact with positive cases.
Meanwhile, there is no clear criteria for when to close a department or an entire hospital. Under previous regulations, if there were two positive cases among the medical staff, the hospital would be immediately closed, a nurse at the major Guangzhou hospital told Caixin.
It is reasonable to close and sterilize a department where infected staff work for a short period of time, and it is beneficial to find close contacts as soon as possible and protect vulnerable groups, Peking University First Hospital’s Wang said. But once sterilization is completed, medical services must be opened immediately, he said.
Hu Bijie, director of the Department of Infectious Diseases at Zhongshan Hospital affiliated to Fudan University in Shanghai, stressed that emergency departments should never be closed.
How should hospitals deal with shortages of medical staff? The international approach is to shorten the quarantine requirement for medical workers. In Germany, vaccinated medical personnel who are in close contact with infected people do not need to be quarantined. Those who are infected need to be quarantined for five days, during which other medical staff take over their shifts, Lu Mengji, a professor at University Hospital Essen’s Institute of Virology in Germany, told Caixin.
The US Centers for Disease Control and Prevention previously recommended that infected medical workers stay home for five days. In January, when Omicron hit the health systems in multiple states, many hospitals allowed asymptomatic positive medical staffers to return to work. Whether well-protected positive medical staff could be in contact with patients who had severe diseases was decided on case-by-case basis.
An even smarter solution might be to allow asymptomatic positive medical staff to directly serve positive patients, Wang said.
He also suggested that construction and expansion of designated hospitals and makeshift quarantine centers has become meaningless. “Omicron is highly infectious and spreads too fast, and the speed of expansion [of quarantine centers] will never keep pace with the development of the pandemic,” he said.
“To fundamentally ease the shortage of medical resources, we still need to promote hierarchical diagnosis and treatment so that mild and asymptomatic patients can be managed at home,” Wang said. “At the same time, all hospitals, whether designated or not, may need to be prepared to accept Covid patients when the winter peak approaches.”
Lack of ICU beds

Fever clinics are full of patients and cross-infections between patients and doctors have begun to emerge.
PHOTO: REUTERS
The key constraint on China’s medical system is the lack of beds in intensive-care units. A 2020 study by the Organization for Economic Cooperation and Development showed that China had 3.6 ICU beds for every 100,000 people, compared with 11.4 in Singapore and 25.8 in the US.
In 2021, the central government set a target to increase the number of ICU beds to 10 per cent of all hospital beds in major cities from less than 3 per cent. Caixin learned that the target has yet to be met, although many hospitals have expanded their ICUs over the past year.
One cheaper, more flexible solution might be the temporary transformation of regular beds into ICU beds, adding electrocardiography monitoring and mobile ventilators, a Guangzhou infectiologist suggested. Based on his experience in the diagnosis and treatment of the current outbreak, many severe patients admitted to hospitals require less oxygen therapy than early patients in the 2020 Wuhan outbreak.
Among infected people, 99.5 per cent may not need to go to a hospital, but the health-care system must ensure that the remaining 0.5 per cent can get hospital treatment, Zhang Wenhong, a prominent infectious disease expert in Shanghai, said in a Covid-19 home recovery handbook released Dec 8.
This story was originally published by
Caixin Global
.


