If Singapore had not initiated measures such as contact tracing and quarantines, more than 5,000 people here would have been infected with Covid-19 by now, instead of 313 as of yesterday.
The outbreak would have hit its peak by July, after which the number of infections here would start going down, said Associate Professor Alexander Cook, vice-dean for research at the NUS Saw Swee Hock School of Public Health.
But Prof Cook explained that for Covid-19 to reach its peak when there is no vaccine available means that half the population - or about 2.9 million people - would have been infected.
Covid-19 is more transmissible than influenza, he said. In the case of flu, one infected person generally passes it to 1.2 to 1.5 other people. For Covid-19, one person transmits it to two to 2.5 people.
Prof Cook is the school's domain leader for biostatistics and modelling, and has been helping the Government with projections of various scenarios in the current crisis.
He said modelling is a simplified representation of reality. But he was quick to add that a model of what has happened so far may not be an indication of what will happen in the future.
Based on the premise of one Covid-19 patient transmitting the infection to another two, the number of people infected doubles every week if nothing is done to disrupt the transmission.
By July, half the population would have been infected. After that, the rate of transmission would naturally slow as there would be fewer people left to infect.
In medical jargon, this is known as herd immunity. That happens when a large number of people recover from a disease and become immune to contracting it again. This serves to break the chain of transmission to others.
But it can be a risky affair.
It is fine to rely on herd immunity to protect segments of the population for a mild disease that rarely kills, such as the H1N1 flu pandemic in 2009.

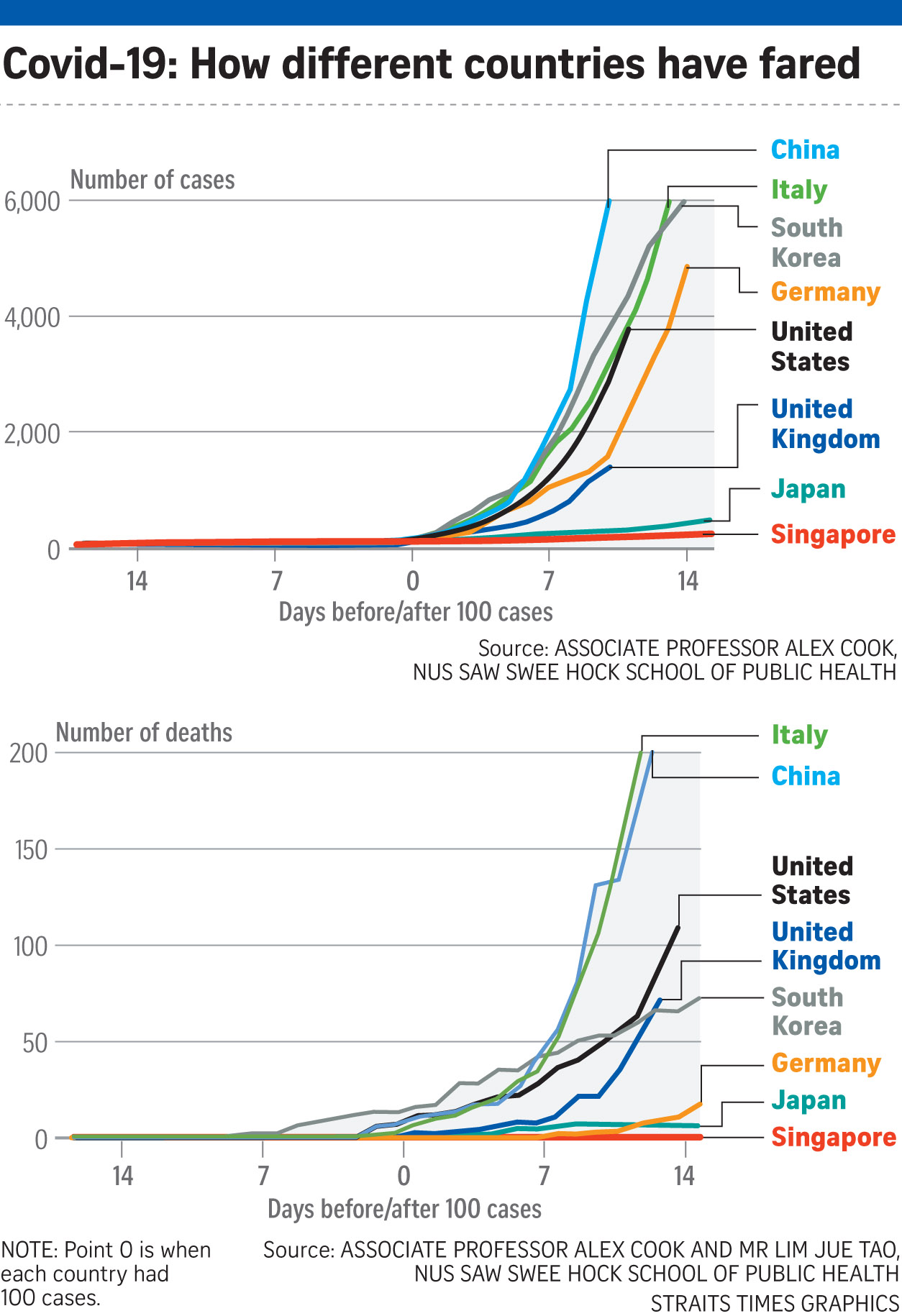
But for Covid-19, the global case fatality rate now hovers around 4 per cent. The case fatality rate varies, at more than 7 per cent in Italy to under 1 per cent in South Korea.
These rates suggest that relying on herd immunity could result in a large number of deaths before the disease is reined in. That is why, Prof Cook said, Singapore should continue to try to contain the disease for as long as possible.
"Right now, cases are sufficiently low, so the Government is able to put a lot of effort into contact tracing," he said.
This, together with other measures such as border checks, has reduced the transmission rate of the disease from the global average of one person spreading it to two to 2.5 other people, to a patient spreading it to just one other person here, he said.
Every day's delay in quarantining someone who is infected can increase the number of cases by 0.15 to 0.2, said Prof Cook.
"It is not much, but it all adds up. If your transmission rate is just above one, you will still get quite a big outbreak."
This is why Singapore tries to identify all the close contacts of an infected person within 24 hours.
Prof Cook said contact tracing to contain a disease is possible with 20 to 30 new cases a day, but added: "You won't be able to do the same level of contact tracing if you have 1,000 cases a day."
Even at that point, he said, contact tracing and quarantining can reduce the overall numbers.
"If we stop our measures, it will go on to the trajectories of other countries. It is going to grow, no way we are going to stop that," he said. "The success is dependent on both the Government and the people acting socially responsible."
This means people observing precautions and the Government continuing with its measures such as contact tracing.
"It is a lot of work," Prof Cook said. "If you miss some, that is okay. Even if you are missing a lot, contact tracing will still bring down the number of cases."
He added: "For sure, we are missing cases." But that does not mean that the people infected by these missing cases will also be missed.
Using contact tracing, it is possible to backtrack and isolate as many close contacts of all those in the cluster. That will minimise the spread and hopefully keep the total number of infections at any one time within manageable limits for the healthcare system.
For now, it is not known exactly how many people have been infected but not identified. This can change the picture as the case fatality rate is different from the infection fatality rate.
Case fatality refers only to identified patients. Infection fatality refers to everyone who has been infected, including those who were not identified when they were sick, or were infected but did not become sick, but are now protected from the virus and will not pass it on.
A team from Duke-NUS Medical School has developed an antibody test that can check if people have been infected and recovered.
Prof Cook said Singapore plans to do a serology study to find out if there are many unidentified people who have had Covid-19.
Looking beyond Singapore's shores, Prof Cook touched on Britain's announcement last week that it was going to allow herd immunity in the population to deal with the outbreak. Britain has done a U-turn since, but the Netherlands has recently indicated it might consider this approach.
The virus appears more deadly to older people and those with underlying diseases. So, Britain wanted this group to self-isolate while enough healthier young people got infected and recovered to provide herd immunity to protect the rest.
Prof Cook said Britain's healthcare system struggles every winter with influenza.
The idea was to overcome Covid-19 in summer. Otherwise, it could push up the number of people dying in winter when those hit with influenza and those infected with Covid-19 fight for the limited healthcare resources.
The plan was "either extremely pessimistic or realistic", Prof Cook said.













