Patients with hypertension fared better in trial that involved fewer pills, counselling from nurses
Sign up now: Get ST's newsletters delivered to your inbox
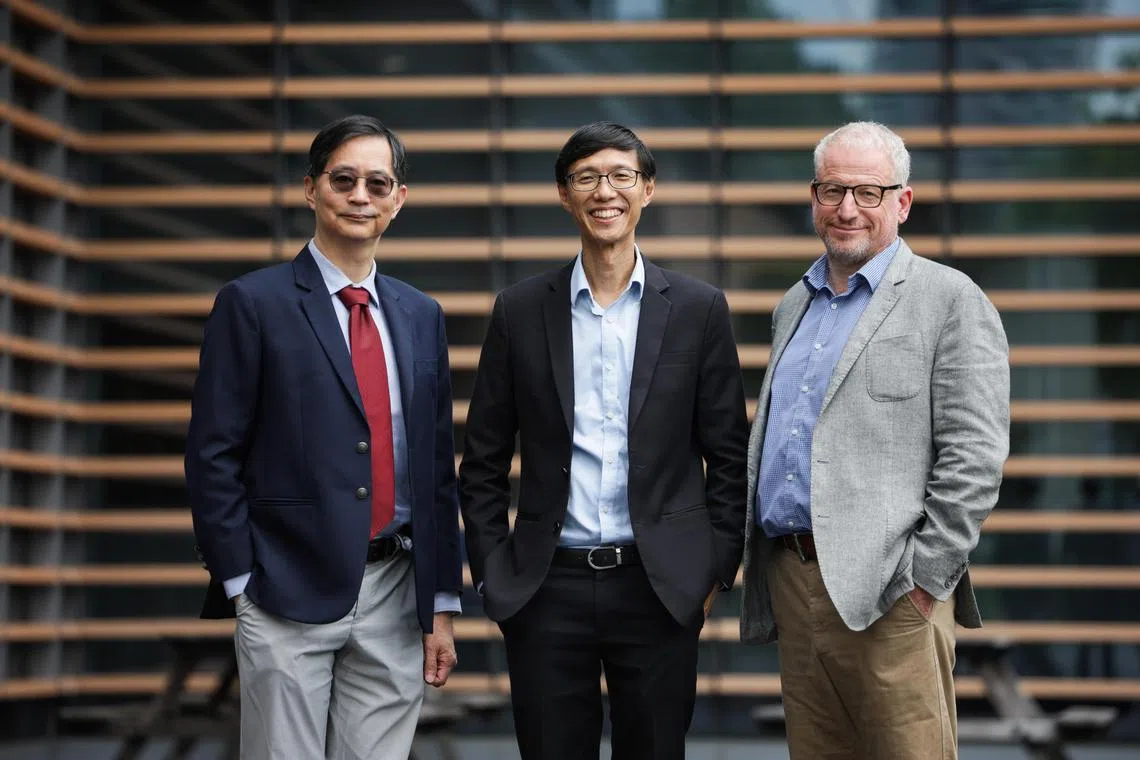
(From left) Professor Patrick Tan, dean-designate, Duke-NUS Medical School; Professor Marcus Ong, Director of Health Services Research and Population Health (HSRPH) Programme at Duke-NUS, and Professor Nicholas Graves, Deputy Director, HSRPH Programme at Duke-NUS, announce the rebranding of their key research programme to focus on population health.
ST PHOTO: GIN TAY
Follow topic:
SINGAPORE - More than six in 10 patients with hypertension saw their blood pressure drop to healthier levels when they had fewer pills to consume and received nudges from nurses to maintain lifestyle changes.
This is an improvement of about 10 percentage points, compared with other patients.
These are some of the results of a trial of more than 900 patients conducted by Duke-NUS Medical School and SingHealth Polyclinics from 2020 to 2022.
A poor rate of patients remembering to take all their medication and their difficulty in sustaining lifestyle changes are common issues, which often lead to poorly controlled blood pressure, and hence a higher risk of patients suffering a stroke or cardiac arrest.
The trial aimed to tackle these issues with the prescription of a single two-in-one anti-hypertensive pill instead of two or more such drugs, as well as getting polyclinic nurses trained in motivational counselling to encourage patients to sustain lifestyle changes.
Around 61 per cent of the patients in the treatment group saw a decrease in their blood pressure to healthier levels of less than 140/90 mm Hg (millimetres of mercury).
In comparison, almost 50 per cent of patients in the control group, which had the conventional course of more medication, and no counselling from nurses, saw a decrease in blood pressure
In addition, more patients in the treatment group saw a reduction in their 10-year cardiovascular risk. The difference between the dip in 10-year risk for the treatment and control groups is also at around 10 percentage points.
The research teams believe that it would be rather easy for the current primary care system to adopt the care model in the trial, and also at a low cost.
They estimated the monthly medical cost at about $20 for each patient, which would include both the cost of the two-in-one pill as well as the counselling and follow-up calls from the nurses.
Although the cost is higher than the $3 to $4 that a Singaporean would pay for subsidised hypertension care at polyclinics, the longer-term impact of the trial’s approach is better, said Professor Tazeen Hasan Jafar of Duke-NUS’ Health Services and Systems Research (HSSR) Programme, who is co-lead investigator of the trial.
Prof Jafar also said the out-of-pocket cost could eventually go much lower for patients with government funding, such as subsidies.
In conjunction with Duke-NUS’ celebration of the 10th anniversary of the Health Services Research Institute, it also announced the rebranding of the HSSR Programme to Health Services Research and Population Health Programme from Oct 1.
Duke-NUS shared that the change in research focus to population health and technology-based research is in response to the challenges faced by Singapore’s health system, including rising healthcare costs, an ageing population, and the growing burden of chronic diseases.
Under the rebranded programme, the medical school will launch new master’s and PhD courses, to develop researchers’ capabilities in population health research.

