Lapses in infection control were behind the hepatitis C outbreak at Singapore General Hospital (SGH) earlier this year, an independent committee reviewing the incident has concluded.
The lapses were compounded by the fact that the kidney patients in the renal ward had weakened immune systems, making them more susceptible to infections.
In addition, the renal ward moved from Ward 64A to Ward 67 in April. The different layout in Ward 67 may have accentuated the gaps in infection control, the committee found.
Its conclusions followed two months of investigation into how the outbreak occurred and whether there were gaps in work processes at the hospital.
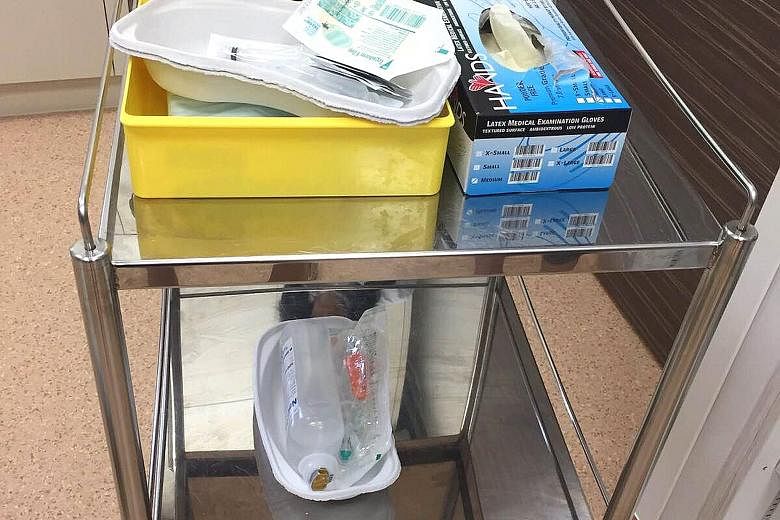
During its review, the committee found small blood stains on medical carts and trolleys used by hospital staff for procedures such as blood- taking and medication administration. Stains were also found on equipment such as an injection tray, as well as on the wall of the "clean" room in Ward 67 where medications were prepared.
-
Boosting infection control
-
This is a summary of the Independent Review Committee's recommendations on infection control.
• Review how ward procedures are carried out to reduce the risk of contaminating the environment or cross-contaminating clean supplies.
•Set aside a clean area to prepare intravenous medication. Items used for invasive procedures are considered contaminated and should not be taken into the area.
•Avoid contaminating equipment or surfaces. Staff should be aware of precautionary measures they can take, such as using washable keyboard covers and not touching surfaces on medical carts with gloved hands.
•Medical equipment such as dialysis machines and computerised medical carts should be comprehensively cleaned.
•Nursing and housekeeping staff should be aware of their clearly designated roles and responsibilities when it comes to environmental cleaning.
•Consistently practise hand hygiene and proper use and handling of supplies for administering injections, such as syringes and needles.
•Improve the current framework for supervision and monitoring, to make sure staff comply with standard operating procedures.
•Extend the recommendations to all healthcare institutions and have the Health Ministry oversee the implementation.
One sample from the wall was taken on Nov 2 - well after the hospital had tightened its infection control measures - and tested positive for the hepatitis C virus.
The committee noted in its report: "The computerised medical carts and procedure trolleys can be possible sources of infection transmission as they are moved from patient to patient.
"During the demonstrations of procedures, it was observed that the computerised medical carts were not adequately cleaned after the procedures."
The committee also observed that staff pushed the carts and trolleys into the designated "clean area" of the preparation room after they were used in procedures, without cleaning them. This would have created opportunities for cross-contamination of clean supplies and medication.
Some ward staff were also seen to have removed the cap of a patient's intravenous cannula when injecting medication, rather than using a side port.
This would increase the risk of a patient's blood flowing out through the cannula, possibly leading to environmental contamination and transmission of infections.
Committee member Lim Seng Gee noted that these practices occurred after the staff were briefed on the inspections at the wards, and it was difficult to know what their practices were like during the hepatitis C outbreak itself.
"When we interviewed them, the practices seemed to be good, but of course that may not have been the case at the time when the outbreak was occurring. It's very difficult to know exactly what went on."

In the report, the committee also highlighted inefficient work processes, which it said could have been a contributing factor in the infection control lapses. This could have been exacerbated by the relocation of the renal ward from Ward 64A to Ward 67, where most of the infections occurred.
In Ward 64A, which has a more compact layout, the preparation room is in the centre of the ward.
In Ward 67, staff have to walk a longer distance between the place for preparing medications and procedures such as blood-taking, and patients' beds.
"The workflow process issues opened up potential for modified infection control practices among ward staff", the committee noted, as not everyone might have followed hygiene protocols.