Cancer of the cervix is one of the most preventable and treatable of cancers.
A regular Pap smear test every two or three years should catch it in the early, or even pre-cancerous, stages, where treatment is straightforward, side effects are few and the prognosis is very good.
It usually takes more than 10 years for the damaged cells to change from pre-cancerous to full-blown cancer.
Because more women are getting screened - in 2012, 70 per cent of women had a Pap smear - the incidence of cervical cancer has fallen drastically to be the 10th most common cancer in women. In 1970, it was second, after breast cancer.
In cancer deaths among women, it ranks eighth, underscoring the need for continued outreach to women to get themselves screened.
Dr Lisa Wong, a gynaecologist in private practice who specialises in women's cancers, expects to see cervical cancer fall off the list of the top 10 cancers in women in the coming years.
This is especially if more young women get vaccinated against it, reducing their risk by 70 to 80 per cent, she said.
Cervical cancer is usually caused by the human papillomavirus (HPV), which is generally transmitted sexually.
There are more than 100 types of HPV, with only about 15 that cause cancer by triggering abnormal growth in the cells in the cervix, the neck of the womb connecting it to the vagina.
The majority of HPV are harmless, though some can result in genital warts - skin growths on the genitals that can cause pain, discomfort and itching.
While the HPV strains 16 and 18 are not that common, they account for 70 to 80 per cent of cervical cancer cases. The two vaccines in the market protect against these strains, and can be paid for from Medisave funds, up to $400 per account per year.
But since other HPV strains not covered by the vaccine can also cause cancer, even women who have been vaccinated should have regular Pap smears, said Dr Wong.
Dr Tay Eng Hseon, medical director of Thomson Women Cancer Centre, said Pap smear screening has "shifted most of the disease detection from cancer to pre-cancer".
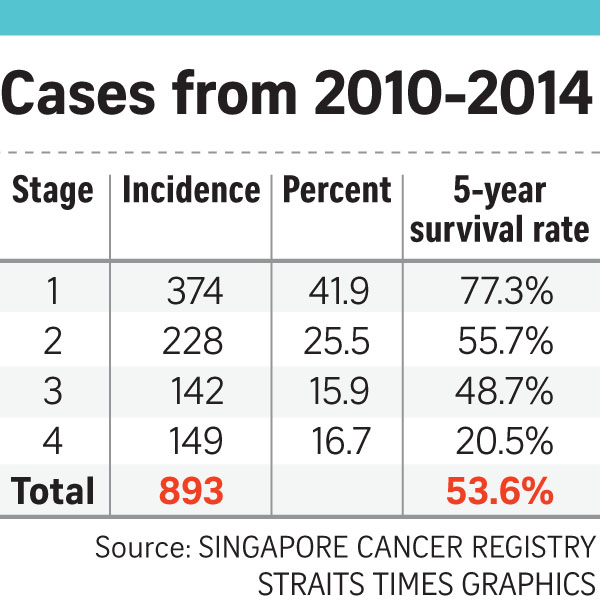
But about half of women who have cervical cancer find out only in the advanced stages, when the cancer has spread, he said.
He said any woman who has had sex, even if only with one partner, should have regular Pap smears. The cost of the test outweighs its benefits only for those who have never had sex, or are over the age of 70 and have had only normal Pap smears.
In addition, there is now a test to check if women have been infected with HPV before, said Dr Wong.
Although it is more expensive than just a Pap smear - she charges $150 for doing both and $60 for just the Pap smear - women who do not have the virus can wait to do their next Pap smear in five years, rather than the originally-recommended two to three.
And even in women who have HPV or pre-cancerous cells, Dr Wong said she is more likely to monitor them than give immediate treatment, as in 80 per cent of women, the issue will clear on its own within a year.
Pre-cancer refers to abnormalities in the cervical cells that are non-malignant but could become cancer after a decade or more.
Because of the long lead time, doctors prefer to treat only the more severe pre-cancer, since the procedure of removing the abnormal cells raises a woman's risk of miscarriage in future pregnancies by about 15 per cent.
If cancer in the cervix is discovered in the early stages, the cancerous part of the cervix can be surgically removed, followed by chemotherapy and radiotherapy to mop up any cancerous cells that might have been left behind.
Removal of the cervix raises the risk of miscarriage in the future by 20 to 30 per cent, Dr Wong said.
If it is discovered in the late stages when the cancerous cells have gone beyond the cervix, possibly to the lungs, bone or lymph nodes, then surgery is pointless, said Dr Wong.
The main treatment in this case is radiation, with chemotherapy used to increase its effectiveness.
Side effects from the chemotherapy tends to be mild, though the radiation could damage surrounding tissues like the bladder and the intestines.
Dr Wong said: "Side effects such as diarrhoea, loose stool and blood in the urine are mild but tend to be permanent."
facebook.com/ST.Salma
•For more information, contact: supportgroup@singaporecancer society.org.sg or call 6499-9147 or 6499-9132; National University Cancer Institute, Singapore on 6773-7888 or e-mail ncis@nuhs.edu.sg
•Next week: Ovarian and uterine cancers.
Find out more about cancer and how to fight it on ST's Fighting Cancer microsite.



