Mrs Tan, 59, was in a tremendous amount of pain when she came to see me. She complained of back pain and pain radiating to her right leg, causing numbness.
She could walk for only 100m before needing to sit and rest. But sitting was not much better, as she could do it for only about 15 minutes at a stretch.
It was better when she was lying down, but the pain flared when she turned from side to side.
She had not slept well for a few nights because of the pain.
Mrs Tan had suffered from chronic back pain for a long time. But this was the first time she had experienced a severe aggravation of pain.
She saw many doctors and was given painkillers and muscle relaxants, but these did not help to alleviate the pain.
She also went for physiotherapy.
After six sessions over a two-week period, her pain lessened by about 20 per cent.
She was told that she needed open surgery because her spinal disc had degenerated.
She hesitated as she was worried about the risk of paralysis and possible nerve injury. She did not want such surgery nor the long convalescence period associated with post-operative healing.
A friend recommended acupuncture and traditional Chinese medicine herbs.
She then tried magnetic treatment - pasting small magnets over her back, and also traction and infra-red heat treatment.
None of it had alleviated her pain by much.
I ordered a magnetic resonance imaging (MRI) scan of her lumbar spine.
This is often thought of as the holy grail for diagnosing the cause of chronic back pain. However, the difficulty is in matching the MRI findings with the symptoms that a patient is suffering from. Sometimes, investigations can be over-interpreted, leading to over-treatment.
About 20 per cent of lumbar spine "abnormalities", or "slipped discs", discovered on MRI scans may just be normal changes in line with the patient's age and physical status.
Some studies show that up to 30 per cent of disc abnormalities may cause no symptoms, and that the person would not have any functional disability.
Hence, we had to be very careful in diagnosing Mrs Tan's condition and determining whether it was actually a mechanical spine problem.
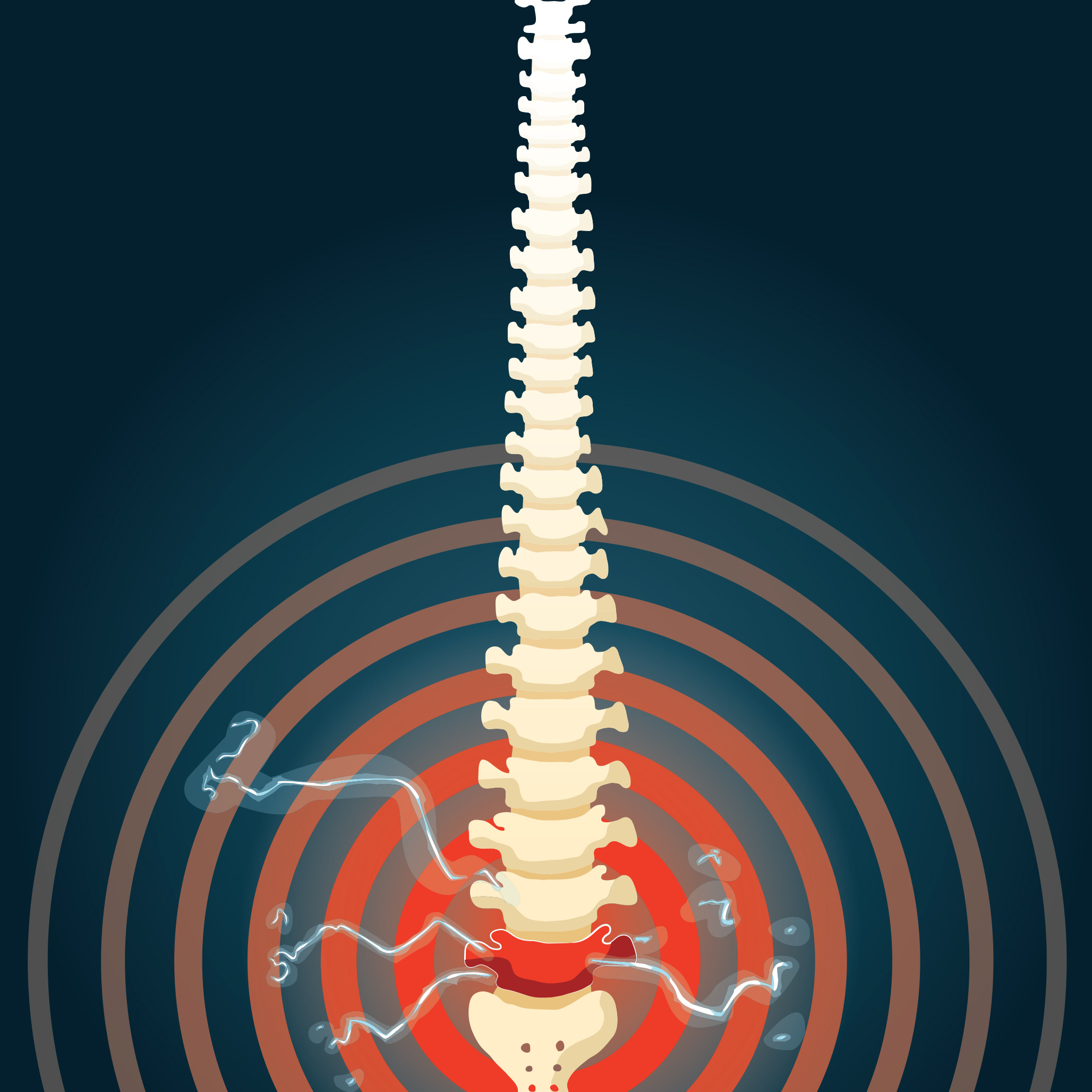
A review of her MRI lumbar spine showed an L4/5 disc degeneration with protrusion of the disc. There was also spinal canal narrowing, which was impinging on the right L5 nerve root.
Mrs Tan's MRI findings matched her physical condition, and were consistent with the right L5 nerve root irritation.
We tried conservative treatment with specialised medication (nerve stabiliser) to treat the nerve root irritation.
There was no improvement in her condition, although she did have more restful sleep at night.
I then offered her either a minimally invasive procedure or open surgery. The minimally invasive procedure would use specialised needles to decompress the spine. It is targeted at the herniation (protrusion) of the disc in order to reduce the pressure within its centre, causing a decompression and subsequent shrinkage of the disc.
Together with a ballooning dilatation technique, we can then free the compressed nerve without any nerve injury.
Alternatively, she could have open surgery to decompress the spine. This is the traditional method of opening up the spine and removing the L4/5 spinal bone in order to reach the disc.
Open surgery has a higher chance - up to 90 per cent - of shrinking the disc and freeing the nerve.
The minimally invasive procedure has a lower chance of shrinking the disc - 80 per cent.
The worst outcome for open surgery is failed back surgery syndrome, meaning the pain will persist after surgery. The incidence of that happening is as high as 25 per cent.
The minimally invasive procedure has a higher chance of providing pain-free results - from 70 to 95 per cent.
Mrs Tan weighed the pros and cons of both options and chose the less painful one.
Having no risk of paralysis and no "down-time" during the recovery phase won her over. Another advantage was that the minimally invasive procedure could be done under regional anaesthesia.
During the procedure, the disc was reduced via a needle decompression and the catheter was able to free the affected nerve.
The procedure took an hour. She was discharged a few hours later, and could walk on the same day.
She underwent a rehabilitation and exercise programme without suffering any more pain.
However, while minimally invasive treatments are popular and effective for the treatment of certain "slipped discs", open surgical decompression is sometimes still the only option for certain patients.
These patients have larger "slipped discs" or an abnormal narrowing of their spinal canals by more than 50 per cent.
It can be compared with the need for open heart bypass surgery for those with severe heart vessel blockages when angioplasty will not do the job effectively.
Fortunately for Mrs Tan, she was a suitable candidate for the minimally invasive procedure and did not have to suffer the after-effects and longer recovery period of open surgery.
•Dr Bernard Lee is consultant pain specialist and director of Singapore Pain Care Centre at Paragon.

