For over a year, going to sleep at a reasonable hour at night was a challenge for 16-year-old Ng Shi Hao.
Before 11pm, he would switch off his mobile phone, turn off the lights and get into bed.
But, hours later, he would still be awake, falling asleep only at about 1am or 2am. Less than five hours later, at 5.30am, he would wake up and get ready for school.
Then he would doze during the 45-minute bus ride to school.
But those naps did not help. He would fall asleep in class and could not concentrate on his studies.
This carried on from about September last year to about the same time this year, when a concerned uncle urged him to seek help at a sleep clinic.
Shi Hao said: "I was preparing for my N levels. He thought I should get my sleep pattern back to normal so I can concentrate on my studies."
He went to the Singapore General Hospital's (SGH) sleep disorders unit and was diagnosed with delayed sleep phase disorder (DSPD).
This condition affects the timing of sleep, and some overseas studies suggest that it affects about one in 10 teenagers.
It is most common in adolescents and young adults whose "night owl" tendencies delay the onset of sleep, often until 2am or later.
Shining some light on sleep therapy
The person will not suffer sleep deprivation if allowed to wake up late. However, early waking times can lead to daytime sleepiness and impaired work and school performance, say doctors.
DSPD is one of many sleep disorders that are sending more people to seek help from sleep clinics here.
The SGH sleep disorders unit has seen a 20 per cent rise in the number of patients over the past three years, said Dr Leow Leong Chai, a consultant in the hospital's department of respiratory and critical care medicine.
Among them are those with circadian rhythm disorders. These are disruptions to the internal body clock that regulates the daily cycle of biological processes.
He sees one to two such patients a month and this group of disorders includes DSPD, which Shi Hao has.
Dr Leow recommended bright light therapy for Shi Hao. With this therapy, the patient sits near a bright light source as prescribed.
The therapy works by influencing the "master biological clock" behind the eyes.
This clock, which consists of a group of nerve cells in the brain, is recalibrated each day in response to external cues - predominantly light exposure, said Dr Leow.
Therefore, exposure to bright light can adjust the body clock, making one feel more awake.
SGH started offering the treatment last December. So far, five patients have undergone it with varying degrees of success.
"I believe we are currently the only hospital doing this," said Dr Leow.
Over at National University Hospital (NUH), about one patient with circadian sleep rhythm disorder is seen each month, said Associate Professor Khoo See Meng, a senior consultant in the division of respiratory and critical care medicine.
But Dr Leow believes the number of patients seen is just the tip of the iceberg. "Many may not know that they can be helped," he said.
At NUH, the patient is usually offered advice on lifestyle and behavioural changes. He is asked to wake up at a fixed time and expose himself to natural light.
Light treatment is often combined with the use of melatonin, a chemical that controls the body clock, said Prof Khoo.
Dr Leow pointed out that not many people can wake up and avail themselves to natural light by sitting outside or near a bright window.
For bright light therapy to work, the brightness must be at 10,000 lux (a measurement of brightness). This is equivalent to outdoor light just after sunrise. By noon, outdoor brightness hits 100,000 lux. Indoor light is usually only about 180 lux.
Patients undergoing bright light treatment should use only units specifically designed for it, said Dr Leow. General lamps may not be bright enough and may not filter ultraviolet light, which can be harmful.
Most studies indicate that early morning treatment, before 8am, is optimal for night owls. The light exposure helps them to stay awake in the day and fall asleep earlier at night, said Dr Leow.
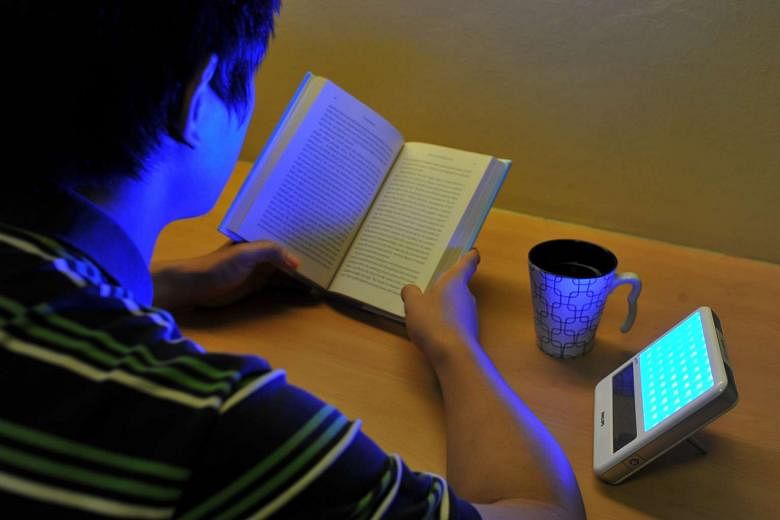
The typical treatment regimen requires the patient to sit comfortably in a quiet setting about half a metre from the light unit, which is usually set on a table at an angle.
Patients can read or have breakfast during the half an hour required in the regimen.
The regimen must be followed consistently every day for patients to see results, said Dr Leow.
An Australian study of 49 adolescents with DSPD showed that at the six-month mark, 82 per cent of those who did not receive any therapy continued to have DSPD. But the figure was only 13 per cent for patients who had bright light therapy and counselling.
Shi Hao used a light box, loaned to him by SGH, for half an hour every day for a week, turning it on after waking up and placing it near the side of his face while he ate breakfast or read.
"Teenagers are advised to bring forward their sleep by one hour every two to three days while using the light therapy," said Dr Leow.
Teenagers should also sleep more. But the early school start time is one of the main culprits for teenagers being sleep-deprived, he added.
The National Sleep Foundation in the United States recommends eight to 10 hours of sleep a night for young adolescents, seven to nine hours for those aged 18 to 64, and seven to eight hours for those over 65.
However, sleep expert Michael Chee, director of the Centre for Cognitive Neuroscience at Duke-NUS Medical School, said seven to eight hours a night would be a more realistic target for older teenagers.
Professor Chee has given talks in schools about the importance of having enough sleep to function optimally when awake and to avoid health issues later in life.
He said some teenagers are concerned that they are not getting enough sleep, but many continue to go to bed late.
Most night owls do not have DSPD, he said. They just prefer to sleep late, and are able to sleep and wake up earlier if need be.
Some teenagers, however, want to buck the sleeping-late trend, get more sleep and lead healthier lives, he added.
Shi Hao is one of them. After a week of bright light therapy in September, he was falling asleep by 11pm. He no longer falls asleep in the bus or in school.
"I am relieved. It helped me to prepare for my N levels, which I have just completed. I want to keep to this sleep pattern as I am hoping to take my O levels next year," he said.