When Emperor Hirohito of Japan ascended to the throne in 1926, his subjects revered him as a descendant of the sun goddess and believed he had divine powers. He died on Jan 7, 1989, of duodenal cancer which was first diagnosed in September 1987.
His doctors lied to him about the actual diagnosis and kept him in the dark throughout his illness. After the emperor's death, his chief physician expressed publicly that he didn't regret not telling the emperor the truth.
In 2012, the medical journal Health Affairs published a paper with the provocative title Physicians Are Not Always Open Or Honest With Patients.
This was a survey of nearly 2,000 doctors in the United States, which found that more than one in 10 of them had specifically told a patient something that was not true in the one year before they were polled.
Of these, more than half had deliberately prognosticated the outcome of an illness in a more positive light than what the clinical evidence indicated.
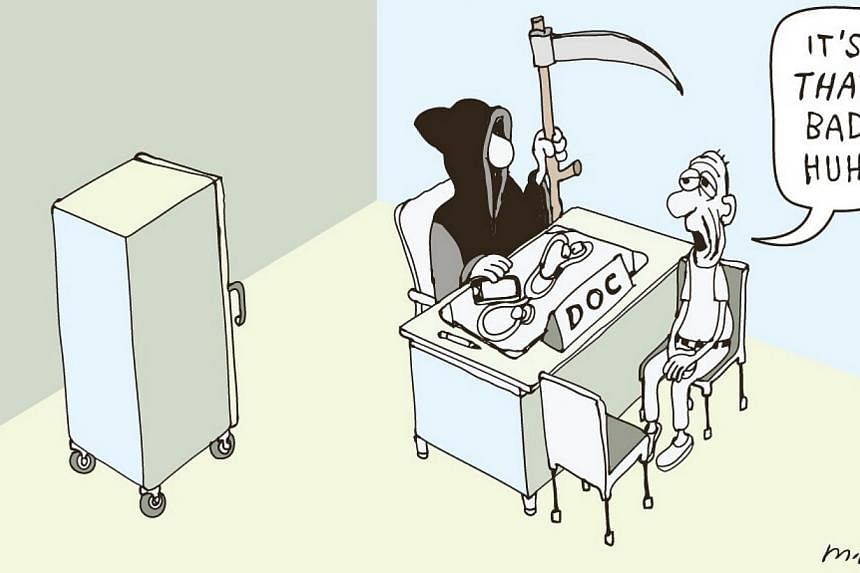
In the not so distant past, it was common practice among doctors to not disclose the diagnosis of an incurable and terminal illness. This sort of medical paternalism was justified on the premise that the truth might hasten the patient's demise by compounding his distress or plunging him into a state of utter despair and even driving him to suicide.
The American Medical Association's code of conduct in the mid-19th century held it as a "sacred duty" to "avoid all things that have a tendency to discourage the patient and depress his spirits".
When Franz Kafka had tuberculosis (in 1924, when there was no cure for TB and being infected meant certain death), he wrote to a friend from the sanatorium where he was to die two months later: "Verbally I don't learn anything definite since in discussing tuberculosis… everyone drops into a shy, evasive, glassy-eyed manner of speech."
Patients empowered
BUT in the past few decades, there has been a shift - at least in the West - from such exercise of paternalism among doctors, to making patients the ultimate arbiters of their own health.
This is based on the ethical principle of patient autonomy which holds that patients should make their own informed decision about their health. Lying to them is wrong as it would impair their ability to make informed choices about their own health.
Studies have shown that an overwhelming majority of patients want to be told the truth even in the face of a serious or terminal illness, and feel frustrated and betrayed when they find out that they had been misled.
In The Death Of Ivan IIych, Leo Tolstoy writes of the anguished dying of the main character amid his family and doctors: "What tormented Ivan IIych most was the deception, the lie, which for some reasons they all accepted, that he was not dying but simply ill, and that he only need keep quiet and undergo a treatment and then something very good would result… This deception tortured him - their not wishing to admit what they all knew and what he knew, but wanting to lie to him concerning his terrible condition, and wishing and forcing him to participate in that lie."
And there are other compelling arguments for telling patients the truth.
Patients seem to do better if they have a full understanding of the illness and treatment, tolerate pain better and require less drugs - provided the truth is told to them in a humane manner.
The bedrock of the patient-doctor relationship is trust. Lying to patients undermines if not destroys that trust. It also corrodes faith in the medical profession and taints future interactions with the possibility of duplicity.
Repeated lying can also have a deleterious effect on the doctor's moral decency. Each lie makes the subsequent one easier to tell and, insidiously and imperceptibly, lying becomes habitual and mendacity becomes second nature.
Tough to be truthful
BUT if truth be told, it can be difficult in the practice of medicine to be totally truthful all the time.
Good doctors care deeply for their patients. Most would want as far as possible to spare them physical and psychological pain and would occasionally find it hard to resist the temptation to give hope even if there seems to be none.
In an op-ed piece in The New York Times following that 2012 article in Medical Affairs, associate professor Danielle Ofri of the New York University School of Medicine commented wryly that she was "amazed that the number of less-than-truthful instances was so low".
She narrated her experience with a patient, an impoverished young woman with a serious heart disease. Her only chance of survival was a heart transplant, but because she was an "undocumented immigrant" this was almost impossible. While knowing that she ought to be open and honest with this patient, Dr Ofri still baulked and couldn't bring herself to tell her the truth.
Like Dr Ofri and probably like many of my fellow doctors, I find that strict and unreflective adherence to the principle of patient autonomy is difficult.
Medicine is rife with uncertainties. Diagnosis can be difficult. Prediction of a disease's outcome can at times be rather treacherous and each patient is unique.
Sometimes, we wonder if a patient is able to grasp at once the truth of the whole complicated situation surrounding his or her disease, without being mired in confusion, distress and indecisiveness. And we always fear that a patient may choose unwisely when faced with distressing news.
This can be seen as mere sophistry but that's how it is with the real-life dilemmas that doctors face. So in some cases, we stall, and parcel out the truth - all the while gauging what and how much the patient can take.
The situation can be made even more complex by another factor. It is not uncommon for relatives of terminally ill patients to ask the doctors not to reveal the diagnosis to the patients.
It seems to be a common enough situation for the Singapore Medical Council to make provision for it in its Ethical Code and Ethical Guidelines.
Section 4.2.4.2 of the ethical code states: "There may be instances of a patient's relatives asking that the patient not be told that he has a fatal or socially embarrassing disease. A doctor may not withhold this information from the patient unless the doctor determines that this is in the best interest of the patient. Doctors shall recognise the role of the family in the decision about whether to disclose a diagnosis to a patient and address their concerns adequately."
Two years after my father's death, my mother developed a malignant brain tumour. It started and grew aggressively in the frontal lobes of her brain. The cancer wiped out her awareness of her illness but left most of her other cognition largely intact. My siblings and I deliberated and, rightly or wrongly, we decided that we would not even attempt to tell her that she was terminally ill.
The devouring cancer changed part of her personality but it spared her any real discomfort and pain right up to the end four months later. Like the chief physician who attended to Emperor Hirohito, I don't - even to this day - regret not telling my mother.
But here's the rub - as a doctor, I am still uncomfortable about not telling patients their diagnosis.
I would be profoundly conflicted should the relatives beseech me to keep it a secret from the patient. And personally, I would not want to be lied to or have any information withheld from me if I were a patient, even if the illness is terminal.
That's how I feel now. Should that day come, I hope that I will have the strength and fortitude to face the bleak truth - and that my doctors will respect my wishes and tell me the truth.
The writer is vice-chairman on the medical board (research) at the Institute of Mental Health.